It’s a sad day when you reach Part Three in a series exposing the popular preoccupation with berating breastfeeding. Yet instinct and experience tell me this won’t stop at a trilogy.
If the previous instalments (
Part One and
Part Two) made you reach the end of your tether, you’ll need to find a lot more tether for this one. Much of the ‘advice’ in the following books smells like the diaper of a formula fed baby. It is parent-centric and resentful of babies. It teaches parents how to ‘train’ their babies to become acceptable, or at least, less of an inconvenience. Hold your breath, we're going in.
Baby and Child: Your Questions Answered.Carol CooperWe’ll start the ball rolling with a tame beast; but a beast nonetheless. This book’s greatest sin lies in its misinformation. Rather than having obvious in-your-face contempt for breastfeeding, the book undermines more subtly by force-feeding the reader with incorrect advice. Much of this advice has the potential to completely sabotage a mother’s breastfeeding efforts. The book commences with the chapter: “Feeding Your New baby”. It begins:
“In general, breastfeeding is better, but, as it’s your baby, you must decide which you want to do. Before you commit yourself, there are many points to consider” (page 32).
Tentative start.
Then we are presented with a basic table detailing the advantages of breast and formula feeding. The usual textbook points are made for breastfeeding - antibodies, cheapness, nicer smelling poops, all the usual jazz. However it’s the list of advantages to formula feeding that has me cropping my eyebrow like James Bond. Check these out! Under “Your’s Baby’s Health”, the list of advantages to formula are listed as:
“Your baby’s supply of milk is not affected by your physical health, nutrition or anxieties”.(Yet neither is breast milk, for the most part).
“She is less likely to be underfed”.(Codswallop. A formula feeding mother can easily under-feed her baby when she does not measure the powder properly – for instance, she may add too much water or too little powder).
![]() |
| Image from page 44. |
“Whilst breast milk is superior in many ways, formula milk is higher in iron and vitamin K”.(This is based on the assumption that the more of a vitamin a product contains, the more nutritious it must be; however in fact, breast milk has a perfect blend of vitamins at an ideal concentration for human babies).
“If you are vegetarian, your baby might be less likely to develop a vitamin B12 deficiency”.(A vegetarian or vegan mother does not need to take any special dietary precautions; she simply needs to follow the same diet as any other new mother).
Okay, that's the apparent advantages of formula to baby's health. Now the advantages for mom's health:
“It does not expose your breasts in public places”(What does this have to do with ‘health?’)
“Milk will not leak from your breasts and stain your clothes”(Again, what does this have to do with ‘health’??)
“Your nipples will not become sore or cracked”(Neither do those of most breastfeeding mothers!)
That's it for mom. Then the book presents a FAQ-style section which basically reads as a catalogue of bitch slaps to breastfeeding. Notable examples include:
“Q: If I have large breasts, could my baby suffocate?
A: It’s possible for large breasts to block your baby’s nostrils, making it difficult for her to feed and breathe at the same time. You can press the breast down just above the areola to give her nostrils more space” (page 33)
This is great advice ...if you want blocked ducts and mastitis.
“Q: If I breastfeed my baby, will my breasts sag later?
A: Breastfeeding may have some effect” (page 33).
(I call a big steaming pile of formula-fed-baby’s crap on this one!)
![]() |
| Image from page 188. |
“Q: Can I exercise when breastfeeding?
A: Very vigorous exercise is not recommended; It is said to increase the lactic acid content of the breast milk” (page 39).
(A mother would need to exercise to maximum 100% intensity for her breastmilk to contain a measurable quantity of lactic acid. Besides, there are no known harmful effects to a baby exposed to lactic acid. Next!)
“Q: Is it a good idea to give a bottle of formula as well as breast milk?
A: It can be a good idea to offer a bottle in the early evening when breast milk supply is likely to be low” (page 41).
(It’s true that breast milk supply tends to be lower in the evening – for this very reason your breasts need all the stimulation they can get. Giving your baby a bottle will deter him from suckling at the breast, thus reducing your supply further. It’s exactly like giving your baby a McFlurry then wondering why they won’t eat the fruit bag. In fact, from a nutritional viewpoint it's exactly like that).
“Q: I feel guilty about bottlefeeding.
A: Formula milk is almost as good nutritionally as breast milk” (page 45).
(Yes and Jimmy Savile is almost as child-friendly as Mr Tumble. What? Too soon?)
“Q: Should I start using a pacifier to comfort my baby?
A: Pacifiers are more useful before the age of six weeks”.(You read that correctly – encouraging pacifier use without mentioning the risks to breastfeeding – tut tut, slapped legs all round). Can we move onto something a little more hardcore now? Gurgle.com step up!
Feeding: Solved, from Breastfeeding to First Foods. Gurgle.comWoah, this book mentions breastfeeding on the cover. It must be an authority on the subject! Before we look at the contents, let me introduce the author. Gurgle.com is a British pregnancy and parenting website owned by high-street parenting store Mothercare (
Mothercare is not Code-compliant by the way). Gurgle.com hosts regular online webchats with parenting ‘experts’ and celebrities. Recent webchats have included: Tess Daly (
who advocates that breastfeeding mothers use bottles at night), midwife Vicki Scott (
who works for bottle manufacturer Philips Avent), Myleene Klass (
who coined the phrase ‘Breastapo’), and professional beacon of breastfeeding knowledge, Dr Miriam Stoppard (
who has said that babies with teeth should stop breastfeeding). This list reads like the lineup at a comedy sketch; however this is childcare advice we’re talking about; and it’s targeted at vulnerable new mothers.
The book begins with a chapter titled “Breastfeeding: the lowdown” (or should that be ‘letdown’? ho ho). The contents of this chapter are a vague as the title. First we are given the standard, ‘there-there’, pat on the back to formula feeders:
“Don’t torment yourself with guilt about it, as your baby will still receive all the nutritional benefit he needs from formula milk” (page 10).
Oh really? So why are formula fed babies at an increased risk of cot death, diabetes, ear infections, allergy, etc? If they were on an even nutritional keel with breastfed babies, they wouldn’t have these disadvantages no? Also consider who the target audience for this book is – mothers to be. The message they get from this simple sentence is: if formula fed babies receive all the nutritional benefit they need, why bother breastfeeding? What a great start to the book.
![]() |
| Image from page 22. |
Later we are told why babies are fussy:
“Your baby may become frustrated because he is not receiving the milk he needs to fill up his tummy” (page 20).
Babies have tiny tummies, about the size of their fist, so they need to feed frequently around the clock. The ‘frustration’ the book speaks of may actually be baby’s cue to feed again, as he has processed the milk in his tiny tummy. Yet the book frames it as ‘baby not receiving the milk he needs’. This exploits the common fear amongst new mothers, that their breastmilk is insufficient; a fear promulgated by a bottle feeding culture which prioritises measurement of intake. The fact however, is that most of babies' frustration has nothing to do with hunger. Wanting to feed is
not the main reason babies cry (
Spock 2004). Discomfort, boredom, and the massive shock to their sensory system that is NEW LIFE ITSELF – are more likely causes. Everything is new to babies: imagine landing on a planet where nothing, not even air or shapes or colours, is like anything you’ve experienced before. Imagine you’ve never felt anything on your skin or digested food – you'd cry too! Especially at the end of the day. Babies cry. This is a fact of life.
Speaking of facts, you won’t find many amongst the pages of this book. Nuggets of fiction dressed as fact include:
“When your breasts feel emptier, it’s time to change breasts” (page 23).
![]() |
| Page 51. |
Given the bottle-centric origins of this book, this sentence is hardly surprising. However breasts are not bottles; they do not get ‘empty’. Even when a woman’s breasts ‘feel empty’ - they are not. It is the baby who should decide when to switch breasts, by latching off and being disinterested. Furthermore, at around 6 weeks a woman’s breasts will naturally start to feel emptier relative to the fullness hereto experienced. This is normal. Her body has regulated to meet her baby’s demand. However if the woman in question were to read this book, she would get the impression that her breasts were ‘empty’ and she would panic. This ignorance is what leads many women to quit breastfeeding around the 6 week mark.
Another area of breastfeeding that is commonly shrouded in ignorance is the dilemma of which breast to feed from first. The book answers this conundrum:
“Start feeding your baby from the breast you last fed on; This means each breast will receive the right amount of stimulation to ensure good milk supply” (page 23).
![]() |
| Page 101. |
This technique is called “block feeding” and is only recommended for women with
over-supply. Block feeding slows milk production, and if adopted by women of average milk supply (that’ll be most women then), it can seriously reduce their production. So this book is actively sabotaging mothers, and it even cites “enhancing good milk supply” to justify its advice. Bitch please!
Another of the book’s strategies of sabotage is to frame breastfeeding as shameful, particularly when done in public. It recommends that:
“A shawl or big scarf can help protect your modesty if you are planning on feeding in public” (page 23).
The assumption is that nursing mothers must hide. No other approach is suggested. More assumptions are made on the topic of introducing bottles:
“Introducing your baby to a bottle, if you are breastfeeding, is actually a good idea” (page 32).
Again, the issue here is what is left
unsaid. The book fails to mention the potentially detrimental risk of nipple confusion and reduced supply.
Speaking of reducing supply, if you want a free ticket to breastfeeding failure, why not force your baby to adopt a feeding routine:
“Babies love routines and they’re good for parents too” (page 72).
At this point you may be thinking that introducing a routine to a 6 month old breastfed baby would be fine, as by that point breastfeeding has been established, milk supply has regulated, solids are being introduced, and baby might even be sleeping through the night. Well you’d be right. A routine at 6 months isn’t necessarily going to spell curtains for your breastfeeding relationship, but this book advocates adopting a routine much sooner than that:
“Here is a routine suitable from three weeks” (page 72).
*Three weeks*! You heard me soldier. Your little squaddy has only been out of the womb for 3 weeks, but God Dammit he better fall inline. Take a gander at your instructions:
Gina Ford would be proud.
However needing to get your baby on a strict schedule from the get go is nothing more than a pavlovian myth, and doing so may be dangerous, because her body is not developmentally ready to wait several hours between feeds or sleep periods. It helps to clarify the issue if you think about the learning process that your baby has to go through. In the womb, she was fed more or less constantly; once born she has to learn to accept that there will be times when she feels full, and times when she is empty. This is a big, scary change for her.
If you’ve followed the book’s advice so far, your life probably looks something like this: You see your baby's every whimper as a signal of your dwindling milk supply; you feel your breasts and they feel 'empty'; you block feed and wonder why your baby’s diaper output is going down; you hide under an burqa in public; you introduce a bottle because for some arbitrary reason it's "a good idea"; and finally you shoehorn your baby into a scheduled routine. After all this, you’re left wondering what’s the point, as “your baby will still receive all the nutritional benefit he needs from formula milk”. You’re hanging on by a thread; so you turn the page and begin the chapter on bottle feeding, where you find the final shunt:
![]() |
| Page 55. |
“Formula milk has been rigorously designed to ensure that it supplies the best possible combination of vitamins and other nutrients” (page 50).
Yup. You read it correctly. “The best possible combination of vitamins and other nutrients”. The *best*. I admit, in all my years of academic research, this is a new one to me. As breastfeeding is the normal way to feed your baby, this book is actually elevating formula above breastfeeding, accompanied by a lovely photo of a formula feeding mother kissing her baby on the forehead whilst she administers the breastmilk substitute. The book even has the cheek to advise mothers to:
“Ask your health visitor or GP for advice as they probably have a favourite brand that they can recommend” (page 54).
Oh I bet they do; considering how relentlessly formula companies market to health professionals; and this marketing is completely unregulated, even less so than other print media (see
here). So directing formula feeding mothers to ask their health professional for their favourite brand is likely to subject them to yet more marketing, rather than an accurate medical analysis of the different formulas available.
![]() |
| Image from page 61. |
The next chapter in the book looks at “Common Feeding Problems”. I was pleasantly surprised to see tongue tie being given it’s very own section with three entire pages devoted to the condition. However my pleasant-surprise turned into WTF-surprise, and then to fuck-this-surprise, when I read the closing paragraph:
“Babies rarely need treatment for tongue tie as they tend to adapt” (page 99).
This basically feeds into the misconception held my many misinformed health professionals, that releasing a tongue-tie is medically unnecessary,
thus denying mothers and babies of the treatment that could save their breastfeeding relationship.
Another medical inaccuracy that sabotages mothers is the belief that lactose intolerance is incompatible with breastfeeding. On page 163 the book orders that:
“Babies with lactose intolerance will need to be taken off breast or formula milk straight away and given a special low-lactose formula that is only available on prescription from a doctor”.What the book fails to mention is that there are in fact, two different kinds of lactose intolerance: primary lactose intolerance and secondary lactose intolerance. The first kind is extremely rare and requires cessation of breast or formula feeding. The second kind is the most common and does not require that a mother stop breastfeeding (she will however have to stop using standard formula if she is bottle feeding). Why does the book focus on the rarest kind which requires mothers to quit breastfeeding yet neglects to mention the kind which enables the mother to continue breastfeeding? After all, the most likely scenario is that if a baby is lactose intolerant, it has the most common form of the condition which is fully compatible with continued breastfeeding. The plot thickens...
After rolling my eyes out of their sockets I turn to the next chapter, which is titled, “Starting Solids”. In this chapter we see Miriam Stoppard’s influence wafting around each page like a fart trapped in a conference room. Basically the chapter coaches mothers on how to mis-read their baby’s signals. Growth spurts are not acknowledged; instead they are used as ‘evidence’ that breast milk alone is not satisfying the baby and so they need solid food:
“There are a few simple indicators that your baby might be ready for solids. For example, if she doesn’t appear satisfied by her milk feeds, perhaps waking in the night when she didn’t used to, this can indicate that she is ready to move on” (page 104).
![]() |
| Page 125. |
Suggesting that milk alone does not satisfy babies prays on a weak point in the mechanics of breastfeeding – the fact that you cannot gauge how much your baby is consuming. This isn’t normally a problem in those parts of the world where there are no scales and no doctors; the mother simply assumes the baby is receiving plenty if the child acts contented and looks well and this works well in the vast majority of cases. However we live in a society fixated on measurement and quantifiable results. Combine this with society’s fetish for chubby babies and it becomes clear why premature introduction of solids is so common.
According to the book, another sign that your baby wants their immature guts violated is:
“Your baby will probably give you signs that she is ready for solids; for example, a loss of interest in or complete refusal to breastfeed” (page 107).
In reality, refusing the breast for a prolonged period (known as a ‘nursing strike’) is more commonly caused by teething discomfort, and introducing solids is likely to aggravate the baby’s condition further.
Yet it seems this book will say anything to reduce babies' access to the breast. Take for example, the section titled, “Why does my baby wake in the night?” It maintains that:
“Many babies find it hard to settle themselves back to sleep and get into the habit of nodding off while having that last breastfeed at night” (page 144).
There is no mention of formula-fed babies falling asleep while having their last feed of the night. In fact, falling asleep after a formula feed has the added negative of bottle rot, which is a syndrome characterized by severe decay of the baby’s teeth (if you’ve got a tough stomach, Google ‘baby bottle teeth’). But of course, this is not mentioned in the book, because we’re only bashing breastfeeding here, silly!
A final fist in the face of breastfeeding, occurs in the last chapter, “Helping your child avoid weight problems”. The text asserts that:
“Avoid grazing if you are breastfeeding. Grazing is when a baby feeds at frequent intervals rather than at set times. A baby who grazes could become a toddler or child who comfort eats” (page 201).
Has this book ever heard of growth spurts?? Cluster feeding, or ‘grazing’ as the book calls it, is an
essential survival mechanism. It is designed to stimulate the mother’s breasts to produce more milk. ‘Grazing’ usually occurs at night, which makes it particularly irritating to parent-centric mommies and daddies. Fortunately for them, a wide range of ‘Sleep Training’ books are available to put a stop to the all-night milk buffet. Oh, here comes one of them now!
Sweet Dreams Arna Skula 2012The title, ‘Sweet Dreams’ suggests tenderness and contentment. However, there’s certainly nothing sweet about this book, particularly its attitude towards babies (aka irritating, inconvenient little tyrants!)
The back cover lists all the highly coveted accomplishments the book promises:
“Correct your baby’s sleep timings and rhythms”(i.e. babies’ are to be ‘corrected’),
“Teach your baby to fall asleep alone, day and night”(i.e. teach them that no one gives a fuck about their needs),
“Use the specially designed charts to see what’s normal at any age”(i.e. babies are robots who can all be programmed to adhere to an arbitrary norm).
But where does breastfeeding come into this? Although the book focuses on babies’ sleep (or rather, how parents can force their babies to sleep more, sleep quietly, and sleep when it’s convenient), sleep is not an isolated part of a baby’s life – instead it is intertwined with factors like development, personality, and nutrition. The book sees nutrition as yet another factor you can manipulate. However manipulating nature, as any failed breastfeeder will tell you (whether you want to know about it about it or not), almost always ends in tears.
So how does the book go about manipulating breastfeeding? First things first, it maintains that under no circumstance should you co-sleep:
“It’s important to get your baby used to the idea of sleeping in a place that belongs to him, in his own little ‘nest’” (page 17).
Still want to co-sleep? Naughty you.
“You’ll do anything you can to sleep a little longer, even just for a few minutes. You may, therefore, choose to stay in bed to feed (particularly if you are breastfeeding), which can result in your baby spending much of the early morning on the breast and it will be very unclear to him when the day begins” (page 82).
![]() |
| From page 73. |
So, firstly the book wants to deprive your baby of the family bed; Next up, it wants to deprive him of night feeds:
“In general, when it comes to improving or changing a child’s sleep, it helps if someone other than the primary carer (usually the mother) takes care of the child for the first few nights” (page 22).
But Daddy hasn’t got boobs. How will baby feed?
“A breastfed baby has no more need for night-time feeds than a bottlefed baby. The reason that breastfed babies wake up more often at night probably has nothing to do with nutrition, but rather with the routines and habits involved in breastfeeding. It is quite likely that it’s mothers’ own insecurity that is responsible for the higher rate of night-time feeding among breastfed babies” (page 38).
This is dangerous advice. Firstly, it is dangerous because all young babies need night feeds, regardless of feeding method; this is a survival mechanism consequential from having a tiny stomach. Secondly, it is dangerous because the hormones responsible for maintaining milk production are more susceptible to stimulation at night; lack of nocturnal stimulation breaks the milk supply chain. Thirdly, it makes me want to bitchslap the author, which is very dangerous (for her) indeed.
Later on in the book, the author makes a suggestion. Check out this tip:
“Try to skip the midnight feed every now and then and see how long your baby can stay asleep without it” (page 90).
Manipulating a baby’s nutritional needs is not an experiment. It’s not like having a snag in your stockings and waiting to see how long you can get away with it. Babies are vulnerable and wholly-dependant. When their needs are left unmet for a period of time, they freak out and are too young to comprehend that they are being ‘trained’. Furthermore, growth hormone levels are much higher during sleep. Thus, the saying, ‘he seemed to grow an inch overnight’. Growth hormones also stimulate hunger. Waking to feed frequently is the baby’s way of making sure he has enough fuel to do the growing.
Yet not content with merely skipping one feed, the book later suggests going cold turkey and giving up night feeds altogether (I can hear mastitis calling!)
![]() |
| Image from page 62. |
“Babies are usually strong-willed and determined. If your baby is like this, stopping night feeds completely may be an easier undertaking than reducing them little by little” (page 104).
Yet if babies could voice an opinion, they would say, “Nonesense! I’m not ready to handle life on my own, not yet”. And they are right. Eventually babies do learn other ways of comforting themselves and dealing with discomfort. But for now, they are learning about trust and security while feeding at the breast.
Following on from the anti-cosleeping, anti-night-feeding instructions, the book then goes on to order distance between mother and baby:
“If your child sleeps in your room, you should sleep in the living room (or another room). Sleeping in the same room as your child means your presence can easily wake him (even if you are quiet, it is not noise but your presence that is disturbing). If your baby is still breastfeeding, try not to hold him the same way you do when breastfeeding as you put him to bed or when you take him in your arms at night. Hold him facing away from you, or against your shoulder” (page 23).
Later in the book, parents are reminded:
“Don’t make eye contact or talk to your baby. Be as reserved as possible” (page 61).
“Babies are born with the ability to fall asleep on their own, or ‘self-soothe’ as it is sometimes called” (page 73).
This is simply untrue and ignores basic biological fact. For safety’s sake, babies are born hard-wired to awaken, which means that if anything threatens their well-being (such as SIDS) they wake up more easily than adults do. Training babies to sleep too deeply, for too long, too young is not in the best interests of the baby’s development and well-being. Yet the book maintains:
“It’s realistic to expect that, at around two months of age, your baby’s night-time sleep will last about eight hours” (page 82).
Two months! Sadly, that is not a typo, this is an actual deadline, but try saying that to a young baby with an empty tummy!
At two months, most mothers understandably feel they do virtually nothing but feed the baby. Books such as this one, with their fantasy 8 hour stretches, undermine mothers’ confidence. In fact, anthropology shows that prolonged night feeding is actually the norm in most human societies outside Western cultures. Playing tricks to lesson night feeding in the early months only serves to lessen your milk supply, so that baby fails to thrive.
Picture the scene: new parents read this book; then suddenly one night, their newborn baby finds himself moved from his parents’ bed into a dark, silent room on his own (against SIDS guidelines of course). He cries from hunger (and probably fear). When a parent arrives, he cannot see them; his body is held away from them. They don’t talk to him. They won’t feed him. They won’t even look at him. He’s too scared to sleep and no one will reassure him. Does this sound like a recipe for ‘sweet’ dreams? (the title of this book). The fact is that very few newborn babies have the ability to self-soothe.
There are no bad habits at this age; your baby legitimately needs your help to fall back to sleep. One of the best gifts you can give your child is to grow up feeling that bedtime is a happy, peaceful, stress-free time to look forward to every night.
The imagery of a parent reluctantly holding their baby at arms-length suggests two people at odds with each other. Indeed the book frames the topic of sleep as a battle of wills – Baby vs Parents; and the ultimate looser must be the baby, whom is shoehorned into the parents’ desired lifestyle. However being a parent isn’t about adapting your baby to suit yourself; rather, it’s about adapting yourself to suit your baby. This book has conveniently forgotten this fundamental facet of parenting, and instead wages war on babies. Take this example from page 91:
“A baby’s self-image starts to develop right from birth. Your baby perceives himself at first as part of you, his mother. Like most babies, your baby then learns to distinguish himself from you without you being aware of the process. Your baby slowly starts to perceive that he is one individual and you are another” (page 91).
So far, big wow. Nothing controversial there. But then comes this left hook:
“However it can take some time for babies who spend a lot of time with their mothers to make this distinction. If your baby goes for a long time before understanding it, he may start to act selfishly towards you, as if you are supposed to do exactly what he wants. To help your baby learn this lesson, the most important thing is to get others involved in his care” (page 91)
Then we have this gem:
“If your baby cries the whole time you are away, it won’t hurt. It’s important not to let behaviour like this faze you. It’s nothing serious and doesn’t merit any particular response” (page 93).
IN YOUR FACE Stay At Home Moms! (and dads). F-YOU attachment parenting! UP YOURS child development! – is basically what the book is saying. It’s arguing that babies are essentially little bastards that will take the piss given half the chance:
“Your baby has to realise that he isn’t in charge of everything and that the world doesn’t revolve around him” (page 126).
News Flash! Babies
are innately selfish. They have to go through a prolonged period of being dependent on others to achieve the kind of emotional security that is the foundation of later independence. Babies are not ready to move on to the next stage until the needs of this stage are fulfilled. They don’t have the developmental abilities to be independent at this age. This is normal, healthy, self-protective behaviour. However this author gives normal behaviour the finger:
“It’s easier to teach a baby these things before three or four months of age. Around three or four months of age, you will start to notice your baby protesting about certain things more systematically than others. He will start to have an opinion about who puts him to bed and who does various other things for him” (page 93).
“With his burgeoning new skills, your baby now starts to grope towards an answer to the question of who is in charge in your household” (page 104).
![]() |
| Pages 56-57 |
Sadly, these views are typical of Cry It Out fans; but is baby’s crying really about defiance? Or do baby’s cries express real human needs? The CIO club insists that babies cry at night because they
want their mother’s attention, not because they need it. In order for the CIO method to pass muster with caring parents it has to downgrade real needs into mere wants. However, in young babies, needs and wants are pretty much the same thing. And in older babies, wanting to be held could still be viewed as a need – an emotional need for comfort. More worryingly, medical problems can be missed because a baby is left to CIO. The bottom line is that,
babies cry to communicate, not manipulate. Yet this book maintains that babies are very much manipulators, and for the large part, breastfeeding is to blame:
“She knows that only Mommy has milk and so she obviously wants her. Of course, she will just be pushing the boundaries here and needs to learn that although she might prefer one parent over the other to do a particular thing for her, that doesn’t mean that you will always be able to grant such wishes. You need to calmly stand your ground” (page 103).
The misguided resentfulness continues:
“Around four months of age, babies often start waking up more frequently and feeding more at night. At six or seven months of age, this tendency becomes even more noticeable. Those babies who wake up to feed start to explore how far they can push things or, as they might say, “How often will they allow me to feed?” or “Well, if I can feed once, could I maybe feed three times? Why not try?” (page 38).
Reading this you might begin to think of babies are manipulative little demons. How dare they seek human contact and sustenance. They’re taking the piss! Can’t we just shut them in a shoebox for the night?
However if you’ve got any compassion and an elementary knowledge of child development, you would know that the baby in question is experiencing a growth spurt (which typically occurs at 4 months then again around 6 months – the exact periods cited). Baby is not trying to manipulate you, instil control over you, or pwn you in any way. Babies of this age are governed by survival instinct. Furthermore, reducing night breastfeeds is actually
counter-productive to sleep, as naturally occurring chemicals in breast milk that are linked to sleepiness, called nucleotides, reach their highest concentration at night.
Yet the book won’t quit. Two pages later, it’s still droning on:
“Babies who want to feed frequently and in small amounts tend to want to sleep frequently and in small amounts. Bringing more order to a baby’s feeding schedule will often have a positive effect on her sleeping rhythms” (page 40).
Like a Breastfeeding Vs Formula Feeding internet thread, the book is
still fruitlessly labouring on this point, many pages later:
“For newborns, feeding and sleeping are connected, which is why there is a link between regular feeding times and regular sleeping times. A baby who, for example, drinks quite often but never takes very much at a time is also likely to want to sleep frequently but never for very long. If your baby is like this, you may want to lengthen the naps she takes, and it’s easiest to do so by lengthening the time between feeds” (page 77).
So the book is advising that you lengthen the period between feeds, whether your baby is ready or not. It does so again here:
“You can expect your newborn to be able to go three or four hours between feeds. Your baby will stop night-time feeds earlier if you work slowly and deliberately, to lengthen one of her periods of sleep” (page 78).
A book shouldn’t tell you when your baby needs to be fed. We eat when we’re hungry, why should we make our babies wait until it’s ‘time’ to feed? Scheduling feedings too rigidly, too young is risky. One of the most common causes of 'failure to thrive' syndrome is failure to listen to and respond to baby’s feeding cues. Yet the book cites that sleep-training should occur from birth(!), and even babies who weigh as little as 6lbs are suitable candidates! Using a Q&A format, the book introduces us to a poor, knackered factional mother who, like every new mom, is suffering from a distinct lack of Zs:
“Q: My son is a month old. I’ve been told I should breastfeed him whenever he wants, and he wants to frequently. He is almost constantly on my breast in the evenings and all the way up to 2am when he finally falls asleep” (page 80).
All sounds perfectly normal to me. A mother’s supply slightly diminishes in the evening, whilst prolactin levels increase, making evenings the ideal time for frequent nursing (biologically speaking, if not socially). So what advice does the author give to this bewildered new mother?
“A: The first thing I think you should look at is your breastfeeding routine. You said that you have been told to ‘breastfeed whenever he wants’. In fact, you should breastfeed him whenever he needs but sometimes it can be a little hard to work out when a baby needs to feed. The risk is that your baby will start to get fed every time he cries, or almost every time – and he may be crying for many reasons other than hunger. He could also start using you as a pacifier.
It isn’t ideal to have a baby constantly on the breast in the evenings as you describe. Enforce some minimum time that you will hold him – say, an hour to begin with – between feeds. With some babies breastfeeding sessions run together, so that the baby starts spending a long time drinking. If this is the case with your baby, you will have to ration the time that he is allowed to drink.
You say he always falls asleep while breastfeeding. You need to train him to fall asleep on his own. Your baby dozes a lot in the evenings while breastfeeding, and though this is cozy now it is not ideal in the long run. Try to create at least some basic routine for breastfeeding: irregular feeding often leads to irregular sleeping! Let his father look after him in the evenings, even if your baby complains about this – the two of them will be able to work it out.
This advice may seem a little at odds with what you have been told, but hopefully it’s not too confusing” (pages 80-81).
I’m loving the last sentence. It’s almost as if the author knows she’s talking bollocks, so has to excuse herself.
Let me get one thing straight: breastfeeding is nature’s plan for comforting babies and helping them fall asleep. That's why breast milk contains a sleep-inducing protein that helps lull a baby into dreamland.
Just in case your eyes haven’t yet popped out of their sockets in a manner resembling the dude from Beetlejuice, the book continues:
“If your baby has trouble holding out until her next feed, she may find it easier if someone other than her mother tends to her in between. This is especially true for breastfed babies” (page 78).
However, as I’m sure you’re aware (you read this blog after all) when breastfeeding, it is important that the breasts get regular stimulation, particularly during the newborn period when the mother’s milk supply is being established. That’s why babies cluster feed. Another reason, as I mentioned before, is that babies’ tiny stomachs can only hold small quantities, they empty fast and need refilling frequently, whatever their feeding method, but especially when breastfed. However the book is willing to ignore this important physiological fact and seek to ‘train’ babies like they’re competing for Crufts. So what other fact about babies’ bodies is it willing to ignore?
How about babies’ sucking techniques:
“Some parents worry that if a very young baby gets a pacifier, it might promote a bad sucking style and lead to breastfeeding problems. Usually, these worries are unfounded. There are many, many examples of babies whose technique for latching on to the breast actually improves after they start to use a pacifier” (page 48).
Refusing to acknowledge the risk of nipple confusion is a common sentiment amongst health professionals. It’s therefore unsurprising that the author of this book calls herself a ‘clinical nurse specialist’. Contrary to the author’s stance, there is no reason to believe that a babies’ latch should improve after offering a pacifier, and every reason to believe that it would deteriorate. A pacifier is a silicone replica of a bottle teat. It’s understandable that the author would champion pacifiers, given the goal of this book – to get babies to be quiet and stop disturbing their parents. However the author’s advice has the unspoken side-effect of sabotaging breastfeeding. It’s worth mentioning that the photos which accompany this advice show a *newborn* baby crying, then being plugged with a pacifier. The text also refers to “very young” babies.
![]() |
| Image from page 48. |
Later in the book, the pro-pacifier agenda is pushed again:
“If he is breastfeeding, he will start to regard your breast as a pacifier. Being seen as a pacifier is not an appealing fate over the long term” (page 85).
If you think about it, all parents - whether breast feeders or formula feeders, female or male – are pacifiers. It’s a parent’s job, particularly when their children are in babyhood, to pacify their children. This is no bad thing. Soothing and comforting an infant strengthens the bond between parent and child. So even if a nursing mother
were used as a pacifier by her baby, this is a positive process of attachment, not the fate worse than hell that this author assumes. Breastfeeding is not just about food – it’s also warmth, closeness, reassurance, comfort, healing, love… a fact the author of this book is unprepared to acknowledge. This is particularly evident in the author’s response to the next mother's Q&A:
“Q: We’re doing the controlled crying technique and have found that my daughter’s naps have improved a lot. We lay her down and sit with her. However the process takes longer if just I sit with her; then she tosses and turns and cries more” (Page 109)
The reply begins with:
“A: Like most babies, and particularly breastfed ones, your baby makes more demands of her mother” (page 109).
It is not explained exactly why a baby seeking comfort from its mother is a bad thing. It appears the author has a major thong-wedgie over attachment parenting. So, when you turn the page and read that the next parent seeking advice is a mother whom co-sleeps and feeds on demand, you can hear the pantie-elastic snap:
“Q: Our son is eight months old and sleeping in our bed. He breastfeeds whenever he wants, which is quite often. It would be okay if he fell asleep in between feeds, but instead he’s always on the move. He’s taken over almost the whole bed. We thought this might be a good time to try and improve the sleep situation. Can you give us some advice?” (page 112).
Can she!! But of course! The author is more than happy to oblige with the advice. I can’t promise much of it will be sane:
“A: When dealing with very active and headstrong babies, gentleness often fails. When dealing with a determined baby, you have to be very determined yourself and give simple, clear, messages. Don’t let your son see you until you breastfeed him in the morning (outside the bedroom). Then, after his morning feed, he needs to stay awake for 2.5 hours before taking a nap. He needs to go outside to play once a day after one of his naps. I would not breastfeed him just before sleep. You say goodnight to him and Daddy, and leave the house at 7.30pm” (page 112-113).
More advice includes:
“As you yourselves realise, breastfeeding plays a big role in your current problems. Your baby is now too old to learn to breastfeed just once during the night, so you will have to discontinue all night feeds. It is easier for a baby to learn to stop breastfeeding completely at night than to learn to feed just once or twice” (page 120)
“Keep in mind that you’re not giving your son to a stranger, but to his father, and getting through the night together, without breast milk, will strengthen the attachment between the two of them. It’s best if you can stay somewhere else for two or three nights while this adjustment is taking place” (page 121).
“Father should sit by the door in the bedroom and act as if he neither hears nor sees what his son is doing or asking for” (page 131).
Next, we’re treated to a follow-up letter written by the same mother, and you can’t help but feel great sorrow for her poor baby:
“Thank you for your very precise advice. We’re a week into the new approach now. There were very loud protests the first evening our son was alone with his father and he didn’t want to back down, but his father put in his headphones to listen to music, and sat calmly. On the second evening there was some improvement. Since then he has made progress every evening, until last night when he screamed again for half an hour but then slept through the whole night” (page 114).
As you read that, you can almost
hear the poor child’s spirit being crushed. This baby is still young – so young in fact, that it has spent more time in the womb than it has yet to spend in the world. His cry is a form of communication. When his father does not respond to his cries, it lets the baby know that his communication is not important. How soul-destroying.
Despite describing what is basically child neglect, the book encourages the parents to continue, and even to detach further by suggesting that the father go out of sight. Also, it’s not explained why the baby must play outside after a particular nap or why he needs to stay awake for a set time period. Nor is it explained what the parents should do if their baby begins dozing off before that time period is up (match sticks under the eye lids perhaps?) Also precisely why the mother must leave the house remains a mystery, presumably it’s to appease the author’s fetish with distancing mother and child. Think of it as de-attachment parenting.
Other information the book leaves unsaid includes information on the dangers of formula-use. For example, page 52 helpfully states:
“Sleep problems can arise in a baby who has repeated ear infections”.However the text fails to mention that formula-use increases the risk of babies getting repeated ear infections. This information would indeed be helpful, but it is omitted because such information would undermine the book’s whole 'formula feeding equals better sleep' agenda.
If this wasn’t concerning enough, in the “Starting Solids” section, the book then hints that mothers should introduce solids earlier than recommendations maintain:
“The current recommendation is that babies should be given only milk until the age of six months, but it’s important to be flexible to meet your baby’s needs” (page 104).
Sadly, this isn’t the only dodgy weaning-related advice. In the same section, the book recommends that:
“When adding a third solid feed to your baby’s diet, make this in the afternoon if you are breastfeeding and in the morning if you are bottlefeeding. The reason for the difference is that it will help keep your milk production if your baby gets only breast milk in the mornings. You will have a lot of milk when you wake up and can readily put your baby to your breast for the first two morning feeds” (page 104).
This is nonsensical. A mother’s breastmilk supply is naturally low in the evenings, so this is
the time of day when she needs
more breast stimulation, not
less. By giving more solids at this time of day rather than earlier, the baby will be get full and so suckle at the breast less causing a drop in milk supply. There is no reason for the arbitrary distinction between breastfed and formulafed babies with regards to how solids should be introduced.
Yet this book is full of arbitrary advice, which is given, paradoxly, under the premise of making life easier for parents. However when you read the advice, you discover that a lot of it is illogical and unduly complex; not to mention heartless. For instance, a glaring consequence of not being child-led is that the author has to devise elaborate instructions on when, how, and where, to feed:
“Morning feeds can be confusing for babies. If you have recently stopped feeding your baby at night, it is important that you feed her outside her bedroom in the morning. If you feed your baby in her bedroom in the morning and she drops off to sleep afterwards, she might think of it as a night-time feed” (page 106).
![]() |
| From page 105. |
When it comes to separation anxiety (which generally occurs around 9 months) the book handles it the same way it handles every other developmental milestone: with a sledgehammer of not-giving-a-fuck:
“Separation anxiety can start to disturb a baby’s night-time sleep. In such cases, your baby will start to cry in his sleep as if he is scared. We don’t know why a baby starts to do this, but a likely explanation is that he is dreaming about what he experienced during the day or other things that are on his mind. You need to be sure not to do too much for your baby when this happens. Always start by waiting for a moment to see whether your baby stops crying on his own. He needs someone nearby, but no more than that. He doesn’t need to be rocked, given something to drink or any other extra service” (page 117).
The next developmental milestone (learning to stand) is approached by all the delicacy of a monster truck:
“When your baby is put to bed for the night, he may stand up straight away, showing off his new skill. Sometimes it will work to hold your baby down for a moment to get him to fall asleep” (page 118).
No, you haven’t just read an excerpt from A Child Called It. This is real parenting advice, given in a parenting manual - and this book was published in 2012. In a nutshell, this book essentially teaches parents how to break their baby’s will. Gah, it's time to move onto another book. From rough-handling to a rough guide, next up it's...
The Rough Guide to Babies & Toddlers Kaz CookeBefore I start explaining why this book should be turned into pulp, I’d like to point out that it has sporadic moments of genuine humour. For instance:
“Get an electric breastpump. The machine will make a noise (sort of a cross between a sucking noise and a vibrator, from memory, but that can’t be right – you’d sound like a porn movie)” (page 80).
Ho ho. If you opened the book at that point, you’d be laughing. However as you turn the pages, the sound of laughter swiftly turns into the sound of tutting, intakes of breath and sighing; with the expression on your face resembling a cat’s backside. It’s no surprise that the author is a fan of Gina Ford (she recommends Ford’s books on page 127).
At the start, the book wastes no time in setting the scene for what is to come:
“Although this book is pro-kid, it is also very much on the side of parents and carers” (page 4)
No shit.
Take this piece of advice for example:
“It’s always best to let sleeping babies lie” (page 37).
Best for who? The parents? – certainly. The baby? – not so much, particularly when the baby is very young. A newborn can be so exhausted by the transition from womb to world, that they sleep through their body’s signals to feed. Not only is this dangerous to the newborn, but it is risky to the mother’s milk supply. Yet the book reiterates the same instructions later on:
![]() |
| The inside cover. |
“If the baby’s asleep, they probably want to be. Certainly never wake a sleeping baby at 2am for their usual feed” (page 131).
If starving your baby isn’t your thing, the book offers the following reassuring advice: put your head in the sand and get someone else to starve them.
“Sleeping through can be encouraged by having a non-lactating person go in to the baby to try to settle them without a feed” (page 133).
Building on this stance, the book suggests adopting a feeding schedule right from the start:
“Your aim would be to feed the baby every three to four hours during the day and when they wake and cry during the night – unless they wake every hour or two, in which case they may just need a rock back to sleep” (page 63).
![]() |
| Wrap baby like fish & chips. No skin to skin here. p169. |
It’s a fact that demand feeding is the most natural and successful approach to breastfeeding, particularly when it is adopted during the night. Yet demand feeding is not suggested at any point in this 564-page doorstop of a book. Why? My guess is that it is because demand feeding is inconvenient to parents, and particularly to formula feeding parents. This isn’t simply a textbook case of omitting information, the book actually critizises and ridicules demand feeding:
“Although breastfeeding as often as you like in the first weeks will help you build up a constant, replenishing supply of milk, it will leave you a zombie if you wake up every couple of hours to feed the baby. Try to give a complete feed at intervals of three to four hours rather than get the baby used to snacking or top-ups every two hours... Try not to feed every two hours as a regular habit. Be aware that you can get yourself into a vicious circle of feeding your baby little bits too often: you’ll need to gradually extend the time between breastfeeds. I finally worked out my baby wanted a feed pretty much exactly every four hours – which is the case for most babies” (page 63).
In fact, when your baby reaches the ripe old age of 9 months (positively geriatric!) the book believes he should only have 3 breastfeeds per 24 hour period! (page 158).
If this wasn’t bad enough, the book goes from shit to shittier with extra shit, when it prescribes an arbitrary time limit for breastfeeds:
“Eventually you’ll probably be feeding only seven to ten minutes on each breast” (page 64).
Presumably many babies have yet to receive this memo; either that or they are deviant little sods.
“Eighty to ninety percent of milk volume goes in in the first four minutes on each breast” (page 69).
How the heck did she figure this one out? This sentence implies that if your baby feeds for longer than four minutes(!), they are doing so unnecessarily. The book fails to cite where the statistic originates from, presumably it comes from that hefty, over-cited peer-reviewed journal they call Fantasy Statistics. That’ll be the same source that the following came from:
“Anecdotal evidence suggests that older moms, especially those over 40, may have difficulty with supplying enough milk. At this age the reproductive system is winding down and the body produces fewer eggs, so it makes sense” (page 70).
No, it doesn’t ‘make sense’ at all. The book seems fond of anecdotal evidence, but I’ll stick with fact: Lactation is not reliant on a functioning reproductive system. Infertile adoptive mothers can breastfeed. Post-menopausal grandmothers can even breastfeed. Lactation and fertility are not linked in the way the book maintains.
More anecdotal evidence abound when the book broaches the topic of breastfeeding twins:
“If you don’t want to do it, here’s official permission: you don’t have to. Anecdotal evidence suggests moms with twins usually give up in the first couple of months or get the hang of it and go on to feed for a year or more” (page 83)
Geee thanks for your official permission. I’m not sure what mother would abandon breastfeeding based on permission given in an amature childcare book. Perhaps the type of mother who gives the following reason:
“Basically I needed to have my body back” (page 90).
This mother sounds dim. She is going from using her breasts to feed her baby, to using her hands (still her body, I’m sure you’ll agree) to feed her baby. She would probably follow this advice on so-called ‘fast weaning’:
“If you have to wean immediately or relatively quickly (over four of five days) for any reason you may spend a couple of days with rock-hard bosoms. Wear a one-size-too small sports bra to ‘bind’ them” (page 87).
...and get a one-stop ticket to Mastitisville! Breast binding can cause breast damage, blocked ducts, infection, interference with breathing and is very painful. It was mainly practiced in the 1940s and has no place in a modern childcare manual. Endurance of breast binding is just one of a catalogue of burdens this book associates with breastfeeding. Another includes the commonly-quoted suggestion favoured by diet police:
“Eat as well and heartily as you can, particularly if you’re breastfeeding. Special breastfeeding or ‘women’s vitamins’ are probably a good idea” (page 48).
Yeah that's a good idea - if you’re Donald Trump. However for those people who don’t have money to burn, vitamin supplements are unnecessary. This is even true for mothers who are eating for three during tandem nursing, or while breastfeeding during pregnancy! The same goes for flushing your kidneys with water every second minute:
“You need to drink a lot during the day if breastfeeding” (page 65).
So, living perched on the toilet because you’ve drank so much water is good; but farting a lot? Apparently, this is very bad:
“For lunch in hospital they served cabbage and I chose not to eat it because I’d been told that it caused problems with gas in babies: mine was the only baby in the ward not screaming during the night and I had a midwife ask me what on earth I had done to have the only angelic baby on the ward. When I told her she was amazed. I found the following to cause problems: coleslaw, broccoli, onion, cherries, kidney beans, spicy food” (page 76).
So if you have farty-pants, your baby will have a farty-diaper and be very upset. This assumption bares no credence to medical or anatomical fact. Rather, gas is produced when bacteria in the intestine interact with the intestinal fiber. Neither gas or fiber can pass into the bloodstream, or into your breastmilk, even when your stomach is gassy. So fart all you like. Hell, go ahead and fart the hospital down. There’s no need to burden your diet with restrictions.
![]() |
| From page 56. |
On the topic of unnecessary burdens, remember the mammoth list of ‘necessary breastfeeding equipment’ suggested by a book in
Part Two of this series? Well that list doesn’t even hold a candle to the following one. Aside from the usual breast pads, nursing bras, breast pump, and those ‘women’s vitamins’ I mentioned earlier, this book lists the following as ‘essential’ breastfeeding kit:
- “A spare top and bra and spare breast pads in your bag at all times in case you leak those big, tell-tale wet circles on your front.
- Pillows to help you support your baby and your back.
- Hot wheat-filled fabric packs (many are designed for microwave heating) to help the milk come in (or use cold to stop your breasts becoming engorged)” (page 66)
![]() |
| Bottles are a 'necessity'. |
Did you hear that people? You simply ‘need’ a wheat filled sack, or else you had better hang up that nursing bra and slump off to the formula isle.
Along with your wheat filled sack, other equipment you will need include one of those over-priced, cumbersome, eyesore rocking chairs:
“Choose a rocking chair or armchair as your breastfeeding HQ. Next to the baby’s bed is perfect, especially for middle of the night feeds” (page 65).
If the thought of arching over a baby in a cold armchair in the middle of the night doesn’t get you questioning your breastfeeding commitment, perhaps the next argument will get the ball rolling. It includes a list of ‘possible drawbacks to breastfeeding’; the most notable of which is:
“You get short-term memory loss, extreme fatigue and other symptoms such as putting the car keys in the toaster” (page 58).
And this doesn’t happen to formula feeding mothers? In fact, studies show that formula feeding parents have less sleep and their sleep is of poorer quality; therefore they are more prone to fatigue (see
here). This book's laughable presentation of fiction is followed up by an even more absurd list (the book has a fetish for lists) titled: “A Wish List For Easy Breastfeeding”. The list includes “as much rest as possible”, “a healthy diet”, “lots of fluids- but not coffee, tea or gin”, and the pier de resistance:
“Luck: you need to be one of the people who can breastfeed” (page 73).
The book doesn’t mention that only 2% of women can’t breastfeed; instead it leaves the threat of being ‘unlucky’ lingering arbitrarily in the air, like that fart in the conference room I was telling you about. Maybe you’ll fall victim, maybe you won’t. Even if you’re aware of the 2% statistic, the book then gives you a list of scenarios which will prevent you from being successful at breastfeeding (I feel like Santa Fucking Clause reading all these damn lists):
“Some reasons why it might not be a good idea for you to breastfeed”. The list is longer than is medically or sanely necessary, and speaks for itself:
Wait. At least it doesn’t suggest that you shouldn’t breastfeeding in public.
“It’s possibly best for everyone in the first few weeks if you leave a crowded room so that you can concentrate fully on breastfeeding” (page 64).
Oh.
“If you’re out and need to feed your baby, go to a large mall or department store and use their ladies’ or mothers’ room” (page 66).
Okay, okay, we get the point. Our baps are well and truly banished to the broom cupboard.
It’s worthy to note that there is no list titled: “Some reasons why it might not be a good idea for you to formula feed”. Perhaps this is because the publisher set a word limit for this book. Nonetheless, the book finds space to squeeze in some sob stories from failed breastfeeders:
![]() |
| From page 60. |
It reads like The Alpha Parent Facebook Page after an onslaught of DFF trolls, rather than a parenting manual. After dismissing the notion that a mother should try to breastfeed, the book then expands on its defeatist “breastfeeding is no big deal” mantra:
“The first month or so will always be hardest. Expect some hurdles and know that you’ll usually be able to get over them. If you can’t, there’s the bottle, so don’t panic” (page 62).
Dangling a bottle like a carrot on a string in front of struggling mothers; who else does that? Ahhh yes, multi-billion dollar corporations – the masters of breastfeeding sabotage. Whilst this book doesn’t quite measure up to the insidiousness of formula companies, it’s clear the author gets her inspiration (and possibly her Carribbean holidays) from them. For instance, a fact of life is that perseverance is key to breastfeeding, yet this book bends over backwards to deter perseverance:
“The problem with perseverance is that when you’re in the middle of a difficult time, every hour seems to drag and every feed can bring new tension and anticipation of pain and trouble” (page 71).
How optimistic! What a glowing appraisal of breastfeeding! It’s a good job this book has a “Getting Help with Breastfeeding Section”. Shame it lists various sources of support then proceeds to critique them in a needlessly unforgiving manner. Check out its description of La Leche League for example:
“The La Leche League is an international charity aiming to help moms breastfeed, with mother-to-mother support and encouragement, and to vigorously promote breastfeeding. While its campaigning function has undoubtedly helped to make strides in international policy, if you’re not convinced of your personal growth through breastfeeding then its helpline may not be the best for you” (page 78).
No more is said about the folks at LLL. We are simply left with the feeling that we ought not to phone them because we don’t fit the vague prerequisite of ‘being convinced by our personal growth’, whatever that means. Perhaps it’s the book’s way of saying, ‘if you’re not truly dedicated to breastfeeding, don’t phone LLL’, in which case this advice should be applied to every helpline.
And thus ends the breastfeeding section of the book. Good riddance. The next chapter is called “Bottles”, although it only looks at formula feeding.
![]() |
| From page 95. |
The chapter begins with the following opener:
“If you decide to bottlefeed, for whatever good reason, it’s important not to feel guilty about it” (page 95).
Well if the mother wasn’t feeling guilty about it, she probably is now. Good job author lady!
Then the book debunks a few pro-breastfeeding studies, spouts a couple of sob stories, the usual jazz. An orchestra of violins play in unison. Then the author chirps:
“Many breastfed children have allergies and asthma, and many bottlefed kids are absolutely brilliant” (page 96).
Yeah and many babies who are exposed to daily second-hand smoke aren’t huffing and puffing around their baby gyms. Still doesn’t make it right. Imagine, if you will, how bad the breastfed children’s allergies would have been if their body had endured the additional onslaught of formula.
It will come as no surprise that this book has a selective approach to communicating information on formula. It’s very hot on presenting the so-called positives, but shy on the risks. For instance, the ‘anti-SIDS checklist’ (page 40) has no mention that formula-feeding increases the risk of SIDS. Not a sausage.
The ‘Bottles’ chapter has a big phat list (YES! a LISSSSSST! Can you
believe it!) entitled: “Good points about bottlefeeding” (page 96). When reading it, you find yourself waiting for an almighty punchline, but it never comes, because this, my friends, is intended to look like a factual list. Highlights include:
“The kid always gets the same thing (breast milk on the other hand, varies in quality and taste according to a mum’s health and diet).”![]() |
| A carton of formula. From page 192. |
This is true. Formula fed kids get the same meal – at every meal. The book implies that this is a
good thing. Can you imagine any other context in which we would feed our children the same, bland, artificial concoction at every single meal - morning, noon and night, for months on end? We wouldn’t even do this to dogs. At least Pedigree Chum comes in a range of flavours. A breastfed baby, on the other hand, enjoys tastes as varied as our own, thus making them less fussy as they grow older. Anyway, back to this so-called list of positives to bottlefeeding:
“Someone else can feed the baby and enjoy the loving bond and eye contact”.
Yup, because you can’t have eye contact with a baby unless you’re holding a rubber teat in its mouth – go figure!
“Your body is now your own again”.This is the same scenario for the breastfeeding mother. The only difference is that she uses her breasts to feed her baby, whilst a bottlefeeding mother uses her hands to feed her baby. Either way, you need to sit and feed the baby. Sorry to break that to you. Life’s a bitch.
Then we have this monstrosity of a paragraph:
“Many people who fear a lack of bonding when forced to give up breastfeeding are thrilled to find that, in the absence of stress and the faff about faulty breastfeeding, bottlefeeding is a tender time that can be spent quietly enjoying the moment, free from pain or worry” (page 97).
.... until of course, your formula fed baby regurgitates their entire meal on your favourite black jeans, followed by screaming for an hour with colic, before passing a steaming, nutty, repugnant formula poop. Kinda spoils the moment.
Notice the words used in this short paragraph. In just one sentence, breastfeeding is associated with the words: stress, faff, and faulty; whereas bottlefeeding is associated with: tender, enjoyment, pain-free, worry-free. Going by this paragraph, it sounds like the author fell down Alice’s rabbit hole and is viewing the world in reverse.
To build upon the view of breastfeeding as faulty, the book quotes a mother simply referred to as ‘Amy’:
“I didn’t have enough milk for my premmie baby and I was under a lot of pressure from health-care workers for him to put on weight. After realizing that he wasn’t thriving at 12 weeks I tried a bottle on him and he looked at me with absolute marvel that I had finally given him a decent meal” (page 97).
How was Amy sure that she did not have enough milk? What techniques did Amy try to stimulate her supply? What support did she seek? Was her baby in otherwise good health? We will never know the answers to these questions. The book doesn’t say. It is statistically likely that Amy could have successfully breastfed her baby, and as a premature baby, he needed her brastmilk even moreso.
Another poor sod with a premature baby tells her tale of woe:
“My firstborn was a premmie and couldn’t suck. My milk didn’t even come in” (page 103)
Still, I’m sure these mothers will be pacified by the following list (a list you say?) titled, “Things you get from bottlefeeding as much as from breastfeeding”. It’s a relatively short list. Let’s look at each item in turn:
“The baby enjoys the sucking reflex”.True. However a baby at the breast can engage in non-nutritive sucking (i.e. enjoy the sucking reflex without having to consume milk). A bottlefed baby, on the other hand, gets a mouthful of milk with each suck on the teat, consequently overfeeding themselves, stretching their stomachs, when all they wanted was comfort.
“Bonding with your baby”.Yes you can bond while formula feeding - sans the naturally-occurring bonding hormones experienced by mother and baby via breastfeeding. When a baby breastfeeds, because of the release of oxytocin, he learns to associate his mother with all kinds of extra good feelings.
“The feeling that you’re sustaining your baby”.Well no, you aren’t sustaining your baby, are you? – Similac, Cow & Gate and friends are. You're just the delivery guy.
“The knowledge that you’re doing your best for your baby and making sure they’re as healthy as possible”.Lie detector going through the roof with this one!
The book even manages to make formula companies look angelic, by turning their profit-hungry motivation into some kind of drive for scientific advancement:
“The important thing to know is that there are plenty of people who make squerzillions of dollars out of formula, the upside of which is that they have a lot of employees working for their companies trying to make the best formula and get it as nutritionally close to breast milk as they can, with some extras such as iron supplements” (page 98).
The amount of money formula companies’ put into research and development is dwarfed by the money they pump into their marketing budget (persuading parents to feed their precious offspring sub-standard crap from cans takes a lot of sophisticated coercion). Consequently, parents pick up the bill for this hyper-marketing through the inflated prices of formula. Does the book mention this? That’s a rhetorical question, obviously.
As for the ‘extras’, I concede, there is certainly a lot of extra crap in formula that you won’t find in breastmilk – again, this is for marketing rather than nutritional purposes. Each formula company tries to pwn the rest by adding more and more fictional pixie-dust to the cauldron. Whereas every ingredient in breast milk was created by nature to serve a purpose. Does the book mention this? Again, rhetorical.
![]() |
| Parents are directed to a specific formula company for 'more info', on page 107. |
In appears that, in an effort to lick the wounds of Defensive Formula Feeders, the book kneels at their crotch, painting a euphoric image of bottlefeeding, which at times, is nothing short of pure fantasy. Take this assertion from page 99 for example:
“Babies on properly prepared formula are never too fat”.Whatevs. You can follow WHO preparation guidelines to the latter and still overfeed your kid with a bottle. As I said above, babies like to comfort suck, but they cannot do so at a bottle without receiving a constant waterfall of milk into their stomach. Whereas at the breast they can regulate their suckling so that no milk is released if they wish. Not to mention
the imbalance of proteins in formula programmes a baby's body for excessive weight gain. In fact, overfeeding and hyper-protein content are some of the reasons that formula fed babies have been observed to sleep longer. They’re all sluggish and bloated from rich Christmas-banquet-sized meals, as illustrated by this comment:
![]() |
| Illustration from page 160. |
“I found my baby slept better through the night as the formula is thicker and fills tummies better” (page 104).
Read: it forms a curd in the baby’s stomach. Nice. This curd sloshes about for hours in your baby’s tummy, stretching it, producing pain and wind. Consequently, and not unlike the average person after Christmas lunch, baby has to sleep off the effects. He’s too uncomfortable to do anything else.
This inclination towards rest is met with hoots and hollars from formula fed parents, who revel in their liberated evenings.
“The more pressure I put on myself to breastfeed the worse I felt, and in the end I put my babies on formula and never looked back” (page 106).
You go sista!! Nevermind about the risk of allergies, gut problems, infections, cancer and SIDS. As long as you have your precious pee-pees. Speaking of sleep, it’s time for another ‘sleep training’ guide...
The Sensational Baby Sleep PlanAlison Scott-WrightThe only thing ‘sensational’ about this book is how it ever got to print. A typical Amazon review tells all:
“The whole attitude and atmosphere to this book made me feel uncomfortable and as a new mother who is exclusively breastfeeding, it was thoroughly depressing and made me quite upset.”
And another:
“As a breastfeeding mother who looked to this book for help I cried when reading this.”
What’s all the fuss about? Let’s take a look. Firstly, the author, Alison (who has no qualifications medically or otherwise) sets the scene for her ‘down-to-earth’ sleeping plan. She uses vague terms such as ‘perfect baby’ and ‘proper family unit’ to undermine government guidelines:
“I am fully aware that the existing government guidelines on feeding and babycare are set out to promote your baby’s health and wellbeing, but they are not always easy either to implement or to stick to. In an ideal world, we would all exclusively breastfeed, not work, stay at home, raise the perfect baby, have a ‘proper’ family unit, masses of help and support, and never be stressed or overtired. As this is not the case for most of us, my plan, although sometimes ‘bending the rules’ a little, is a down-to-earth and sympathetic approach designed to meet the needs of both parents and baby” (page 2).
So she acknowledges that government guidelines exist to promote babies’ health and wellbeing, and then proceeds to say she will be discarding them because they are inconvenient to parents. So far, nothing ground-braking; Gina Ford has been doing this for years. Then Alison regurgitates another tired-old clique:
“My method is always baby-led and mother-focused, working on the basis that if the mother wasn’t happy then baby wouldn’t be happy either, and vice versa” (page 2).
‘Happy mom - happy baby’ the mating call of the lazy-parent. It is often sung by those who put their own needs first, and want to justify it. Case in point:
“In my view it is better to adopt an approach that can be adapted to your lifestyle than to restrict yourself to a method that you may find difficult to maintain” (page 24).
News flash: fuck your lifestyle. Babies take a steaming big dump on your lifestyle the moment they are born till approximately eighteen years of age. A parent who believes she can shoehorn her baby into her existing lifestyle will soon be shoehorning herself into a straightjacket. Yet somehow the ‘happy mom – happy baby’ comfort blankie continues to be a popular fantasy of many. Take the following paragraph for example, which screams “SABOTAGE” in big Disneyland flashing neon lights. Here, a mother speaks of her experience of being advised by Alison:
“My baby was not gaining weight, I was really struggling with breastfeeding and my baby never slept. Alison came round and after much discussion we gave Margot her first bottle of formula. She sucked it down in 1 minute and then fell asleep for 3 hours. It was a beautiful sunny day – the first time I had noticed in 3 weeks. I had a feeling of complete relief and physically felt my shoulders loosen as the tension flooded out of me. I realised that formula feeding was not ‘evil’ and bad, and that, as Alison had said, ‘a happy mom makes a happy baby’. Margot and I have never looked back...Breast is best, but not for everyone!” (page 24).
Sad indeed is the fact that this mother had her breastfeeding relationship sabotaged by a self-appointed sleep guru with no training in baby-care or anything else. At a time when the mother needed to work on her supply more than ever, formula was given to reduce it further (top ups are also recommended by Alison as an ironic ‘cure’ for supply problems on page 88). This mother obviously set out to breastfeed, yet was manipulated while she was at her most vulnerable, by someone disguising themselves as support. Sadly, when a mother is feeling exhausted, it is easy for a person with an anti-breastfeeding agenda to exploit the mother’s urge for rest.
![]() |
| Another example of covert sabotage, p38. |
Most pro-formula sentiment rests on the empty promise of rest, so it is no surprise that this book rejects demand-feeding:
“The decision of when to feed has to come from the parent and not the baby. Demand feeding is often unmanageable, as parents cannot take charge of their days but are controlled by the demands of the baby” (page 8).
Even newborns, fresh from the womb apparently should have their hunger cues ignored:
“I advise using my plan from Day 1, or at least starting as early as possible” (page 5).
“Most babies are born nocturnal and it is very important to re-train them within the first few weeks of life” (page 66).
Re-train is an interesting choice of phrase. Babies are not performing circus seals. They are born hard-wired for survival. Re-training them means forcing them to go against their natural biorhythms. These physical, emotional and cognitive cycles are central to your baby’s optimum development, however they have one snag – they tend to be inconvenient to parents, who have different biorhythms. Why are babies’ biorhythms so different from adults? Answer: because babies need to sleep this way. Rather than temporarily alter your adult biorhythms to accommodate your baby’s, Alison suggests forcing these alterations upon your immature and vulnerable newborn. For example:
“Persevere with feeds during the day to ensure that your baby takes enough milk to help him get through the night” (page 64).
Eradicating night feeds during the early months with lead to a botched supply, as I mentioned earlier.
Another part of Alison’s re-training process includes giving your baby a bath every day:
“Always introduce an end-of-day bath and bedtime routine as soon as it is possible to do so” (page 117).
Bathing your baby every day, particularly a young baby, will leave them vulnerable to developing eczema and other dermatological problems. This is because bathing washes away the skin’s naturally protective oils. The risk is exacerbated further when any products are used. Yet many parents are fixated with baths as an integral part of the bedtime routine because they have been influenced by companies such as Johnson & Johnson and by health professionals (who have also been marketed to by Johnson & Johnson).
Next, Alison gives your baby a deadline for sleeping through:
“It has become plain to me that young babies are, on the whole, capable of sleeping through the night by around eight weeks of age” (page 10).
Poor little mites. So that means that by 8 weeks, your baby should have zero night feeds. The book features a letter from a mother whose 10 week old baby failed to receive this memo:
“We have been putting our baby to bed around 7pm since Week 1. He is now ten weeks old and still cries for 10-15 minutes before going to sleep, but then he does sleep all through the night. Is this normal and is there anything we can do?” (page 79).
In Alison's reply, she dismisses the baby’s evident distress:
“Really there is no such thing as ‘normal’ – all babies are individuals and will display different behaviour patterns. Although he cries, your baby does eventually go to sleep and then sleeps through the night. This indicates that there is little wrong and I would suggest that it is just his way of winding down as he prepares to sleep. It is fairly common behaviour and nothing to worry about. I would advise little or no intervention to try to stop him crying as this may only disturb him, thus prolonging the time it takes him to go to sleep” (page 80).
This baby’s basic biological cues were not being listened to, and his needs were not being met. So he had given up on trying to connect with his caregivers. Alison repeats the same advice to a different parent later in the book:
“It may seem harsh just to put him into bed while he is so upset, but it is often the best thing to do” (page 91).
Alison maintains that you should follow this cruel isolation approach, even when your baby is in unfamiliar surroundings:
“If your baby sleeps in his own room at home you might feel worried about disturbing his sleep at night while staying in a hotel, for instance. There is little you can do in these circumstances except position the cot in the corner of the room as far away as possible from your bed. You may even be able to put the cot behind a screen, chest of drawers or wardrobe so that your baby cannot see you” (page 92).
Aside from having to sleep alone, your baby is not permitted to feed at inconvenient times, and certainly not to cluster feed:
“A healthy newborn baby should be able to feed well at the breast and then last for a couple of hours between feeds” (page 35).
This load of bollocks would win Oscars. However movie babies aside, the fact is that
healthy newborn babies cluster feed, particularly during one of their many growth spurts. It’s nature’s way of boosting breastmilk production. Yet Alison refuses to acknowledge the existence of growth spurts in this Q&A session:
“Q: I often find that my baby is unable to wait for his next feed. What shall I do?
A: If you are breastfeeding this can be quite common in the first couple of weeks and if you need to offer an extra top-up feed or so during the day just ‘go with the flow’ as this phase should soon pass. However if your baby seems unable to take enough milk at each feed and is therefore consistently unable to fall into the 3-hour feeding plan, then something is wrong and I would advise you to read pages 54-9 on troubleshooting feed problems” (page 103).
Errrrr HELLO! Growth spurts!
No baby, particularly a breastfeed one, should be sleeping through the night by 8 weeks, yet Alison even applies this unnatural standard to
sick babies:
“Even if your baby has been unwell throughout the day and hasn’t taken much feed, it should not be necessary for you to re-introduce a feed during the night” (page 93).
This is tantamount to starvation, not to mention ignoring a sick baby’s increased need for fluids.
Once you’ve starved your ill baby according to Alison’s exacting instructions, whatever you do – don’t comfort him for too long!
“During the night, if your baby develops a slight temperature and appears too hot, give him a dose of Paracetamol and remove a layer or two of bedding or clothing. Do remember that your own body heat will increase his temperature if you hold him closely for too long while trying to comfort him” (page 93).
No cluster feeds, check! No night feeds, check! No long cuddles, check! So when do I need to start this training? Allison maintains that your baby must follow her sleep plan, starting from the get go:
“In the first few days after birth, leave your baby to sleep and feed him only when he wakes during the night” (page 33).
This is a newborn we’re talking about! (tiny stomach). This is your freshly lactating boobs we’re talking about (building supply). It is extremely important that your breasts get night time stimulation, particularly during your baby’s first few weeks (see, ‘
Timeline of a Breastfed Baby’). When you feed during the night, prolactin levels surge to ten times the amount they would during a day feed – this is really good news for your milk supply. The higher the prolactin levels, the more milk you make. New mothers should see night feedings as opportunities to boost their supply – and seize them!
Yet in Alison’s plan, demand feeds are forbidden. In fact, Alison seems to have a warped view of demand feeding, as she equates it with toddler tantrums:
“This is a prime example of where my suggestions go against the accepted guidelines, as I do not believe that ‘demand feeding’ is beneficial to either mother or baby. I fail to understand why parents are encouraged to respond to ‘demand’ from a baby in the first few months whereas a ‘demand’ from a toddler is then deemed to be unacceptable behaviour” (page 8).
“Surely it is you, the parent, who needs to be the one to put the boundaries in place, rather than your baby?” (page 9).
What a conundrum. Contrast the above sentence with the following sentence, found later in the book:
“Your decision of whether to breast or bottle feed may be influenced by jealousy from a demanding toddler who is upset with a new baby” (page 25).
Verrrrrry interesting. So babies, who are governed solely by primitive survival instincts, should not call the shots, but toddlers should? Isn’t it a tad unhealthy to let a toddler dictate how their baby sibling is fed?
I have a ‘radical’ suggestion; instead of framing sleeping and feeding decisions as a Child Vs Parents battle of the wills, how about viewing it as a
team effort; whereby parents help their child to feed and sleep better (i.e. attachment parenting), rather than forcing him to. Alison disagrees. Apparently attachment parenting, demand feeding and SIDS guidelines have produced generations of babies who can’t sleep:
“I believe that sleep problems in babies are escalating due to a number of factors:
- The advice that babies should sleep in the parents’ bedroom for at least the first six months.
- Babies are now placed on their backs to sleep. However, many babies struggle to relax and settle in this unnatural position.
- It is becoming increasingly understood and accepted that many women are now having babies later in life. These older mums often experience higher levels of anxiety and are less likely to be able to leave their babies to settle to sleep without feeling the need to check on them constantly” (page 18).
Woah, generalise some? Actually, studies have shown that younger mothers tend to me more anxious than their older counter-parts (
Corderoy 2012).
Want to know what I think has caused the rise in ‘sleep problems’? Trashy detachment parenting books like this one. There’s a direct correlation between an increase in baby-taming ‘gurus’ flooding the market with their hyper-scheduled sleep and feeding routines, and the increase in ‘sleep problems.’ Why? Because such ‘experts’ have framed perfectly normal infant behaviour as a ‘problem’. You see, the definition of what constitutes a problem depends very much on our expectations. If we expect babies to act as babies, we won’t perceive their natural behaviour as problematic.
Books like this one have a subjective perception of what
they think it means to be a ‘normal’ baby. The trouble is that this perception is often based on an out-dated model, stemming from a time when most babies were artificially fed, slept prone, and slept in isolation.
SIDS guidelines are certainly
not contributing to a so-called influx of infant sleep problems and Alison’s dismissal of the guidelines is tantamount to negligence. ‘Back-to-Sleep’ campaigns have been the biggest breakthrough in lowering the risk of SIDS. In most countries, back sleeping has lowered the risk of SIDS by around fifty percent. Fact.
Regarding said guidelines, Alison maintains:
“I believe it is up to each individual parent and carer to access the advice and information provided and to be aware, as I am, of the guidelines given” (page 80).
Sounds good, but then Alison goes on to say:
“I recently read a very interesting book called ‘The Cot Death Cover-up’ which disproves most of the common risk factors associated with cot death today. It is well worth spending some time to read the author’s proven theories” (page 80).
The book in question, published fifteen years ago, is written by a man called Mr Sprott. He was ignored in his native New Zealand, and so tried his theories out on the British market, and was ignored there too. Basically he argued that cot death has only one single cause – toxic gases created by mattresses. Period. Needless to say, all the major SIDS organisations and Government agencies have discredited his ‘theory’. Nonetheless, Alison uses it to defend her sleep plan.
The plan is very dangerous where SIDS is concerned, as it contravenes several of the most important preventative guidelines. For instance:
“My suggestion is to put your baby in his own room within the first few weeks” (page 76).
“It may seem harsh to be putting your baby to bed on his own from the very early days, but within a short space of time he will come to accept it” (page 77).
Here’s the scoop: closeness, not separateness, is the normal psychological and emotional state for babies. When a baby wakes up alone in a dark, quiet room – behind bars – a sort of ‘What’s wrong with this picture?’ anxious thought process goes on and cortisol levels rise. Persistently high cortisol levels have been linked with the development of learning difficulties and depression (
Sears 2009).
Aside from these mental disabilities, how about giving your baby a nice big dose of death? As well as putting your baby to sleep in a room alone from birth, Alison also advises that you put your baby to sleep on his stomach. She cites ‘flathead syndrome’ as a reason not to follow anti-SIDS guidelines which recommend that you place your baby on their back to sleep. This makes zero sense. Would you rather your baby have a minor and temporary cosmetic condition, or like, be dead?
Of course, the chapter wouldn’t be complete without a glowing fantasy appraisal from a fictional mother:
“Elsa sort of slept through the night from about eight weeks. However, she was on her back and thrashed around in her sleep and was very hard to settle, and she still always seemed so tired. She was diagnosed with reflux and we started a course of reflux medication which helped ease her discomfort, but she was still so restless and uncomfortable during the night. After consulting Alison we put Elisa on her tummy to sleep. Bingo – what a difference! It was amazing to watch her in sleep – I could tell she was so much more comfortable and totally at rest. We never looked back from that moment and it was tummy all the way” (page 83).
This mother was playing a dangerous game of roulette with her baby’s life, and Alison wants you to do the same with your baby. However the facts speak for themselves: babies lying on their backs are less likely to become overheated because back-sleeping leaves the internal organs exposed so that they can radiate heat more easily than when on the tummy (
Sears 2009). Also when sleeping facedown, a baby can press his head into a soft surface and suffocate.
Despite her lack of qualifications, Alison fancies herself not only as baby-trainer-come-paediatric-consultant, but also a nutritionist:
“An important part of successful breastfeeding is making sure that you have a healthy balanced diet with plenty of fluids” (page 38).
A ‘healthy balanced diet’ (purposely vague term) is not a necessary prerequisite to successful breastfeeding. Here, Alison is simply placing an unnecessary burden on breastfeeding mothers. Not many mothers (read: humans) can manage to maintain a balanced diet (5 a day, strict adherence to the food pyramid, all that lark), nor should they be anal about it, particularly in the postnatal period. Yet Alison continues:
“What you should eat while breastfeeding remains a completely individual choice and I usually advise continuing with the same balanced diet that you ate throughout your pregnancy” (page 39).
This, quite frankly, is balls. The diet of a breastfeeding mother definitely does not need to be as restrictive as a pregnant mother’s diet. As we’re on the topic of food, cue one of the most abused breastfeeding myths of all time:
“Certain foods can have a negative effect on some babies and can cause them to be unsettled, have bouts of crying, become very ‘windy’ and have explosive stools, or even vomit. If possible, try to monitor your diet in relation to your baby’s behaviour” (page 39).
The above paragraph is 100% true – if it were written about formula. However in reference to breastmilk it is mere slander. Yes people, Alison is slandering your breasts! In her eyes, your norks are temperamentally-minded toxic waste dispensers. The funny thing (and by that I mean, totally unfunny) is that the foods Alison lists as being risky, are some of the most bland-ass foods in existence: “pasta, tomatoes, and salad” (page 40). And don’t get her started on alcohol!
“Alcohol (especially champagne) should be avoided, as the bubbles almost seem to transfer into the breast milk – result: one very bloated and windy baby!)” (page 40).
This is a sad attempt to downgrade breast milk (Alison says it will give you a windy baby) to the same level as formula (science says it will give you a windy baby).
“If you do happen to have more than one or two drinks, then it is advisable to express your breast milk before you go to bed and discard it, as it will contain a high level of toxins from the alcohol” (page 40).
This is another unnecessary burden. The alcohol will dissipate from your milk at the same rate as it leaves your blood. Contrary to misinformed belief, alcohol does not stagnate in your breasts.
On the medication front, even tame medications such as antibiotics, when mixed with breast milk, are, according to Alison, given a toxicity that would put kryptonite to shame:
“Although many health professionals and doctors advise that it is safe to take antibiotics while breastfeeding, I am not so sure as I have observed a link between the onset of digestive issues in some breastfed babies and their mums taking certain antibiotics. My advice is to read the antibiotic information leaflet and if it lists heart-burn or gastric discomfort as side-effects in the patient, then you can assume that this might cause similar problems in the baby. I would suggest that you ‘pump and dump’ while taking the medication, feeding your baby either stored breast milk and/or formula and resuming breastfeeding once you have finished taking the course of tablets. I will be completely honest here: it may be that your baby will not re-accept the breast after getting used to a bottle for a number of days and you may then have to give up breastfeeding” (page 48).
So let me get this straight. Alison wants you to risk losing your breastfeeding relationship so that you can pump to avoid a non-existent risk. It appears she has seriously miscalculated her readers’ dedication to breastfeeding.
On the topic of unnecessary burdens, Alison creates pointless dichotomies in an effort to put distance between parent and baby. For a start, she argues that feeding and cuddling should never go together:
“All babies learn by association. It is therefore important from Day 1 that your baby learns the right associations and how to differentiate between night and day, feeding and cuddling, playing and sleeping” (page 6).
Then she presents an intricately detailed, three page long, 29 step process to achieving a suitable latch (Yes, 29 steps you must follow each time you latch your baby!) I’m not going to use up bandwidth going through each in turn; suffice to say the usual suspects are paraded: pillow propping, water guzzling, snack setting-up, neck supporting, tummy supporting, shoulder supporting, TV remote locating (yes really), and legs placed at 90 degree angle (get your protractors out ladies!) After this gymnastics lesson, we have the following vague step:
“Try to make sure you are feeling as calm and relaxed as possible – though with sore nipples, the thought of anyone coming near your boobs, let alone getting baby latched on, can make it impossible to feel relaxed!”How helpful.
At this point I came to the conclusion that Allison must be getting paid-per-word for her book, and so dragged this list on for as long as her keyboard would allow. Take for example:
“Step #25: Although you need to concentrate on how your baby is feeding and it is tempting to want to gaze adoringly at him all the time, be careful not to look down continually as it can cause you to get a really stiff neck” (page 43).
Yes, that’s why we see mothers with neck braces lining the corridors of baby groups. Surely this ‘advice’ has no place on a list of how to achieve a sufficient latch, as it is equally applicable to formula feeding mothers (and anyone who likes holding babies – grannies of the world beware!)
Before she moves onto the ‘Expressing breast milk’ section of the book, Alison dishes out some more breastfeeding tips (oh joy!)
“Begin each feed by offering the breast that you fed from last at the previous feed” (page 44).
This is called block feeding, and as I mentioned above, it’s only recommended for mothers who have over-supply. Block feeding when you don’t have oversupply can needlessly reduce your supply; as can this:
“If your baby is simply not interested, or is too sleepy to feed, put him down” (page 44).
And this:
“If you do just miss the odd feed here and there and don’t pump instead, it really should be OK” (page 49).
And this (Cry It Out fans, here’s something for you):
“Each night try to set a target time in your mind that you aim to reach before feeding your baby. For instance, if he has been waking for his first feed anywhere between 11 and 11.30pm for the last three nights, then set your target time as maybe 11.45pm or midnight and keep trying to lengthen the time before you give him a feed” (page 108).
Why does CIO persistently pop up in parenting books like this? One reason is because it appears to ‘work’, at least for some babies. If no one comes to comfort them, some babies do eventually cry themselves to sleep. However a baby who cries furiously before falling asleep will sleep in a state of hormonal havoc. Crying releases stress hormones into the baby’s circulation. Furthermore, listening to baby cry also releases stress hormones in the mother that will prevent her from sleeping soundly. As a result, you have a dyad of anxious insomniacs. To enable the mother to maintain her resolve in the face of her baby’s distress, Alison has created a ‘crying scale’. 1 is the merest whimper and 10 is a ‘full on scream’.
![]()
(page 110).
![]() |
| From page 176. |
Yeah, just take your sweet leisurely time about it and hope that your baby shuts up. And if he doesn’t shut up, remember:
“Don’t panic, persevere for as long as you feel comfortable and if you want to offer a bottle of either expressed milk or formula instead to give yourself a break, then do so – there is no need to feel guilty!” (page 44).
Moms, how about listening to the biological cues of your body when your baby cries, rather than to advisors such as Alison, who tell you to turn a deaf ear. Fascinating biological changes take place in your body in response to your infant’s cry. Upon hearing your baby cry, the blood flow to your breasts increases, accompanied by a biological urge to ‘pick up and feed’. Go-go gadget breasts! The act of breastfeeding itself causes a surge in oxytocin, brings feelings of relaxation and pleasure, a pleasant release from the tension built up by the baby’s cry. These biological happenings explain why it’s easy for Alison to advise leaving your baby to cry – she is not biologically connected to your baby.
Anyway, if you have any supply left by this stage, you might want to try expressing it; and even if you don’t, Alison will push you into doing so, in her section devoted to the topic:
“If you have chosen exclusively to use breast milk for your baby, then it is advisable to try and get to grips with expressing some milk at least once or twice a day. This milk can then be used to replace one breastfeed during the night” (page 45).
Whatever for Alison? Why is it ‘advisable’ for a mother to replace a breastfeed at a time when her breasts need the most stimulation? (i.e. at night when supply is naturally low, and receptive hormone levels naturally high). Also, what about the fact that a breast pump cannot extract as much milk as a baby?
“You may be told that a breast pump is not as efficient as your baby and that pumping will have a detrimental effect on your milk production, but I do not believe this to be the case” (page 45).
In the absence of Alison citing any studies or sources, would you choose to reject La Leche League and trust her on this one? Not if the next gem is anything to go by:
“Introduce your baby to a bottle in the first couple of weeks which will help to avoid rejection of the bottle at a later stage” (page 45).
... and may cause your baby to reject the breast altogether! Far more advisable to wait until at least 4 weeks when breastfeeding will be more established. Six weeks – even better.
Hey, have you noticed, we’ve had a page where Alison hasn’t mentioned the F-word. One whole page!! Cause for celebration! But before you hang out the bunting...
“Some moms find expressing relatively easy and can pump off 90ml in 10 minutes or so, while others can take half an hour just to get 20ml. If you find that you don’t like or don’t get on with pumping but still want to substitute a couple of feeds, then obviously you can use formula” (page 46).
And obviously Alison, you can fuck off. Using formula is not an ‘obvious’ go-to when a mother cannot express. Donor milk is an option, or juggling life choices so that expressing is not necessary. Formula is (or should be) a last resort.
However, as last resorts go, apparently formula is the holy grail; so much so that Alison devotes not one, not two, but six (six!) whole pages of information on how to give up breastfeeding! Then she moves swiftly onto the formula feeding chapter, the introduction of which reads...
“It is a shame in today’s society that formula-feeding, when used in preference to breastfeeding, is almost frowned-upon – to the point of making some women feel that they are ‘bad mothers’ if they choose it rather than breastfeeding” (page 59).
(Imagine an orchestra of violins playing the tune from Titanic as you read that). Alison continues:
“Since its introduction, formula has continued to improve in quality and most types even contain lipids and pro-biotics, making them as similar to breast milk as ever before” (page 60).
Sure, about as similar as a hole in a tree - and my asshole. Listen up people: your breastmilk is nutritionally balanced and has the exact combination of water, carbohydrates, protein, fats, vitamins, minerals, enzymes and antibodies your baby needs. What's more, there are hormones and other growth factors in your milk that make important contributions to your baby's growth and development. Your breastmilk is constantly changing in its composition throughout the day and throughout the course of lactation to meet the changing needs of your growing child. Formula has none of these attributes. None.
Next, we are given an insight into the inner workings of Alison’s brain (an Aladdin's Cave of propaganda) as she ponders aloud:
“I often wonder if human breast milk is the ‘natural’ food it is always claimed to be these days. If you stop to consider the ‘unnatural’ methods used in the production of the foods we eat –genetic modification, over-cultivation, pest control and animal management – how can we be sure that our breast milk remains ‘pure’ and unaffected” (page 60).
What this paragraph is doing in the formula-feeding chapter is anyone’s guess. I’m presuming it’s to lick the wounds of the guilt-ridden formula feeding mother. In any case, can’t Alison see the irony of citing genetic modification, over-cultivation, pest control and animal management in this chapter? These are all mechanisms
directly involved in the creation of formula. We’re not talking somewhere far down the chain like with breastfeeding, where a nursing mother who once drank some bottled water from Wales that a sheep shat in before it was purified. Rather, these mechanisms are part of the formula manufacturing chain
itself. Breastfeeding is the best way to keep babies' exposure to such toxic contaminants as low as possible as they appear to be filtered out by the mothers' body (
Gray and Jamieson 2011). If Alison is suggesting that breast milk is not as ‘natural’ or ‘pure’ as people claim, what superior alternative is she suggesting? (There is none). But she doesn’t stop there.
“A recent article in The Times suggests that much of the recent research promoting breastfeeding over formula is actually flawed. The article highlights the fact that statistics cannot truly prove that breastfed children have higher IQs than those fed on formula, as there are too many other contributing factors that are not taken into account. The main fact is that the majority of babies who are fed with breast milk are known to be born to parents in the middle to upper classes and their children will probably enjoy a higher standard of education. So although the majority of breastfed babies may prove to have better outcomes in life, this could easily be due to factors that were not taken into account when the statistics were compiled” (page 60).
Yawn. This is not a groundbreaking critique of breastfeeding studies. This sort of drivel has been spouted by DFFs since the internet took its first breath in the 90s; but okay I’ll bite. Firstly, this paragraph focuses on only one type of breastfeeding study – those concerned with IQ, yet the paragraph begins, “Much of the recent research promoting breastfeeding over formula is actually flawed” suggesting pro-breastfeeding studies *in general* are flawed. This is a grossly broad allegation which Alison fails to provide any rationale or evidence for. Secondly, I reiterate: what is this information doing in a chapter about formula feeding?? Thirdly, every major study on breastfeeding and IQ
does account for socio-economic factors such as parents education, occupation and income and still finds breastfed babies to come out on top (I'll come back to this later). Finally, a gene has been ear-marked as responsible for the rise in IQ amongst breastfed babies. This gene (FADS2 if you’re interested) is triggered when, and only when, the baby is breastfed. A
gene interacts with the components of breastmilk to preserve a baby’s true cognitive potential. So whilst I don’t deny that breastfeeding mothers are generally more intelligent [*preens*], this alone, is not why their babies tend to have higher intelligence than their formula-guzzling peers. There is a physiological root.
Now that we’ve got that cleared up, let’s move onto Alison’s next assault on fact:
“A mom who has chosen to bottlefeed from the start will build up a bond with her baby the same as any mother who breastfeeds” (page 60).
Yeah sure - sans the intense hormonal bond and codependency that binds the breastfeeding mother to her nursling. Lacking these elements, a bottlefeeding mother
cannot bond on the same level. This is a physiological fact. Noticing the frailty of her argument, Alison adds the following in an attempt to buff it up:
“Also, in my experience it can sometimes be easier to build a bond through being able to maintain eye contact while holding your baby in a bottlefeeding position” (page 61).
A breastfeeding pair are tummy to tummy, skin to skin, a perfect alignment which lends itself to prolonged eye contact.
Sadly, the assault on fact isn’t confined to breastfeeding, Alison dishes out a toxic smorgasbord of formula feeding falsehoods:
“There are new guidelines in place with regard to making up feeds, as there is some concern that, once opened, a box of milk powder is then not sterile and should be added to hot water to kill any bacteria” (page 62).
Almost correct; but when we’re taking about the safety of babies, ‘almost’ just isn’t good enough. In reality, formula powder is not sterile, even when the box is sealed (by law it has to state this on said box). Alison’s comment suggests that powder from a freshly opened box would be sterile if used straight away, and this is simply not true. But wait, it gets worse:
“I have found the easiest and most practical way – which is still, in my opinion, safe – is to prepare and store bottles ahead of time” (page 63).
She then gives a 7-step procedure for making up bottles in bulk and then storing them in the fridge.
“I suggest that you have enough bottles that you need only wash, steralise and prepare them once a day” (page 63).
These instructions will no doubt appeal to those mothers who chose formula feeding because it taps into to their lazy inclinations; however the detriment to their babies could prove fatal.
Speaking of laziness, many mothers choose to wean their babies onto solids earlier than the 6 month World Health Organisation guideline in the hope that their babies will sleep longer and thus stop being irritating in the night. Alison feeds this false hope by giving the go-ahead on early weaning:
![]() |
| Notice the bottom paragraph. |
“Q: My baby is 4 months old and from nine weeks old he has been sleeping through the night without waking or feeding. Suddenly he has started to wake at night at around 2am and is sucking his hand as if hungry. Should I offer him a feed?
A: Babies can be unpredictable and, despite having been settled in a routine for several weeks, their habits can for some strange reason suddenly change” (page 111).
Yeah, it’s called a growth spurt. In fact, one occurs at 4 months. Anyway, you were saying?
“...We may never discover what causes these changes, but in this case it could be due to the fact that your baby is hungry and not being sustained through milk alone” (page 111).
*headdesk*
I'm getting tired and stressed out reading this shit. But wait, Alison says this will effect my supply:
“The extent of hormonal changes occurring in your body during lactation means it can be an extremely emotional time. When you put your baby to the breast oxytocin and prolactin encourage milk production. However, if you are feeling stressed, overtired, anxious, or tense, the production of these hormones can become suppressed” (page 33).
What new parent doesn’t get stressed, overtired, anxious or tense? These are integral emotions of new parenthood, particularly during the newborn phase. Every parent will feel them at some point, so does that mean that every parent will have supply issues? That’s the conclusion Alison wants you to make. And what’s her solution? Well, it may have formula written all over it:
“Understanding this emotional cycle may help you to continue breastfeeding successfully by knowing when to take a break, whether perhaps to supplement a feed with formula, and when to get some much-needed rest” (page 33).
Diamond. Get a break by using a more inconvenient time-consuming feeding method. Go figure!
But it gets worse, much worse:
“During the first few days after birth it may be difficult for you as a new mother to believe that your breasts will produce sufficient nourishment for your baby. They may still be soft and unchanged, and you may not see any evidence of colostrums production. Today’s guidelines do not advocate giving any milk supplements to your baby during this early stage, but I suggest that each new mother and baby should be treated as the individuals that they are and each situation assessed accordingly. If you feel that your baby is hungry, unsettled and crying even after having what you assume to be a substantial feed at the breast, don’t be afraid to offer a supplemental feed if you feel you need to do so” (page 35).
Babies cry for many reasons (as illustrated
here), most of the time it has nothing to do with hunger. Yet here we see the seed planted that a woman’s breasts are inefficient at the job of breastfeeding. Next Alison, waters the seed, giving a not-so-subtle nudge to formula:
“Do remember that if you are struggling with your breastfeeding, feeling under pressure and are beginning to dread each feed, there is always another option. You have the right to choose and try out another method without being made to feel guilty” (page 35).
Then she puts some fertilizer on the seed:
“Milk insufficiency is the most common reason for mothers to decide to give up breastfeeding” (page 35).
Alison missed a vital word here: milk insufficiency is the most common reason *cited* for mothers to decide to give up breastfeeding. Most women are led to think they have insufficient milk by insidious agenda-pushing idiots like Alison. Take, for example, this worrisome advice:
“Become ‘breast aware’. Before feeding, feel your breasts; then do it again after the feed. This can help give you some confidence that your baby has had a good feed, as your breasts will feel softer and less heavy after feeding than they did before you started” (page 43).
A mother’s breasts begin to feel
permanently soft and even ‘empty’ at around week 6. This coincides with a drop in pumped amounts. To the novice breastfeeder, these appear to be signs that her milk is drying up, and it is this fear that Alison is exploiting. However feeling soft and empty is actually the
normal physiological state for lactating breasts. At the same time, a mother may stop leaking or may stop feeling let-down (or feel it less). This means that her body has figured out how much milk is being removed from the breast and is no longer making too much. Her breasts have regulated and are now in perfect harmony with her baby.
However Alison omits this vital information. Rather, once the seed of doubt has been planted, and tended to, Alison administers the final push towards formula:
“Other common problems with which many breastfeeding mothers struggle are: an inability to achieve a good position or latch; becoming so overtired that the quantity and/or quality of their breast milk are affected; being given poor advice on breastfeeding schedule; the suggestion to feed on demand; or a digestive problem, such as reflux, from which the baby may be suffering” (page 36).
Not once is it mentioned that
all these problems can be resolved. Also notice the comedy moment: “being given poor advice on breastfeeding schedule”. Yup, it appears Alison is even citing herself as a prime source of breastfeeding anguish. Notice also the reference to reflux. Yes Alison has a thing or two to say about this topic:
“We all know the saying ‘breast is best’, but actually I believe this is not always the case for some babies with reflux. I have read and understood all the theories supporting this statement, and on the whole it may be true, but through my work I have been unable to ignore the fact that sometimes breast is *not* best when dealing with this condition. I do understand that many mothers have a strongly emotional and deeply rooted desire to breastfeed and feel devastated and inadequate if unable to do so or if faced with the prospect of having to give up. There are many different opinions on whether breastfeeding actually makes the symptoms of reflux easier for the baby to deal with, or whether breast milk can aggravate the symptoms” (page 221).
There’s a reason why reflux is less common in breastfed babies. No actually, I lie - there’re
several reasons. Firstly, non-nutritive sucking (which can occur during breastfeeding but
not bottle-feeding) reduces irritation and speeds gastric emptying. Secondly, the breastfed baby’s tongue motion triggers peristaltic waves along the gastrointestinal tract, these muscular contractions help the milk and food travel down into the stomach. Thirdly, breastmilk leaves the stomach much faster (so there’s less time for it to back up into the esophagus). Fourthly, breast milk is nature’s antacid, containing enzymes which neutralize stomach acid. In fact, breastfed babies with reflux have been shown to have shorter and fewer reflux episodes and less severe reflux at night than formula-fed babies (
Heacock 1992).
*Aaaaand breathe*
But aside from reflux, poor positioning, poor latch, being overtired, poor quantity, poor quality, poor support aside – aside from these things, breastfeeding is best, yeah? Well, nope. Alison still has one more scenario in which breast is not best - the catch-all category of women; the least likely, yet commonly cited, Miss Malfunctioning Mammaries:
“There are mothers who are physiologically unable to breastfeed or genuinely unable to produce sufficient milk for their babies, and these mothers will be able to substitute formula for breast milk to feed and nurture their babies” (page 36).
Check out the idealised, Hallmark-style language associated with formula-use at the end of that sorry paragraph. Not once is it mentioned that the percentage of women who physically can’t breastfeeding is 2%, probably because if you can persuade yourself that your breasts are faulty, you are on the road to guilt-free formula feeding.
One thing even Goofy could logically deduce so far is – Allison does not want you to exclusively breastfeed. Her plan is incompatible with exclusive breastfeeding (EBF) because EBF requires you to listen to nature, whereas Alison’s plan requires you to deny nature. However approach this presents a problem for Alison: many mothers want to exclusively breastfeed because they want their babies to develop optimally; so how can Alison persuade these mothers to give up their EBF dreams? Simple. Just downplay ALL the benefits of exclusive breastfeeding. Check out this double-page spread; It lists the advantages for 4 different feeding methods (exclusive breastfeeding, pumping and breastfeeding, combination feeding, and exclusive formula feeding):
![]() |
| Pages 26 and 27. |
Notice how combination feeding is said to have ALL the benefits of exclusive breastfeeding (Google ‘the virgin gut’ to understand why this is tush). So why bother exclusively breastfeeding if apparently your baby will get all the same benefits from combination feeding (and have the added perk of getting someone else to do the feeds?) – is exactly what Alison wants you to ask yourself. Also notice how the list of benefits to combined feeding focuses heavily on the assumption that babies are not satisfied without being topped-up with formula; that a mother can never truly supply enough milk for her baby. (It all sounds very Clare Byam-Cook to me; How did the human race ever survive sans formula?)
Notice also at the bottom of the page, it says, “There are some very real advantages to formula feeding”. Fancy a laugh? Let’s turn the page and take look at each in turn:
- Advantage #1: “It is easier to monitor milk intake and see how much your baby drinks”.
To reassure yourself that your breastfed baby is ingesting enough, just check their diapers; it’s not rocket science. Many bottle feeders mistakenly believe that by using a bottle, they can easily measure how much their baby has consumed. This is actually not true. Bottle-fed babies more often regurgitate some quantity of a feed. Short of putting a dip-stick into their puke, there is no way of knowing exactly how much has been brought back up. Also, the increased metabolic workload for the baby, lower digestibility of nutrients, and increased waste inherent in formula, make measuring the benefit of each feed – impossible.
- Advantage #2: “Formula gives longer and more lasting satisfaction to a baby”.
Sure, if you equate satisfaction with being a beached whale. Would
you like to eat the equivalent of a seven-course Christmas dinner for
every meal? Young babies (less than 6 months) have an immature digestive system. Their gastrointestinal tract does not produce digestive enzymes as a child or adult does. Babies can digest breastmilk more easily than infant formula because breastmilk contains enzymes (amylase and lipase) that aid digestion. So whilst a formula-fed baby may feel fuller longer, he is more likely to have more ‘pain in the gut’ from wind and allergies.
- Advantage #3: “Babies with lactose-intolerance can be fed lactose-free formula”.
The same babies could also be fed breastmilk, as the most common type of lactose intolerance is compatible with breastfeeding.
- Advantage #4: “Babies with either cows-milk protein intolerance and/or multiple food allergies can be fed with hypoallergenic formulas designed specifically for babies with these problems”
Ditto above. Breastmilk is best for these babies.
- Advantage #5: “Some babies who suffer from reflux respond better to specially designed anti-reflux formulas than to breast milk”.
Breast milk is the ideal food for reflux babies as it neutralises the acid in their tiny tummies.
- Advantage #6: “Siblings can be more involved and ‘help’ at feed times, hopefully initiating more interaction and acceptance of the baby”.
Siblings can help and interact with a breastfed baby in many ways, as can Dad, Grandad, Florrie the next-door neighbour, your cousin Pete, and the cat. Wielding a bottle does not equate to bonding.
- Advantage #7: “More freedom for the mother, avoiding the feeling that you are only being used as a ‘feeding machine’”.
And there’s me thinking that formula feeding mothers fed their babies too, or do they just leave them to starve? Surely bottle-feeding is more ‘machine’-like than breastfeeding, as it has the mother wielding a man-made device.
- Advantage #8: “Your partner can have much more involvement with feeding your baby from the start”.
Ahhh, but if you’re breastfeeding, you have a prime justification for delegating diaper duty to him (and bath duty, and cuddle duty, and whatever other ‘involvement’ will enrich his relationship). Why the fixation on feeding? (See, ‘
The Laziness Conundrum’).
- Advantage #9: “Less physical or emotional strain than on a mother who is breastfeeding”.
Not true. Emotionally, a formula feeding parent is more likely to feel understandable guilt and unresolved turmoil as a direct consequence of formula feeding. Physically, she can get back ache from lugging all those bottles around.
- Advantage #10: “More freedom with your choice of clothes as you do not need easy access to your breast at all times!”
Yes more fashion freedom – if you like your Ralph Lauren marinated in formula spit up.
- Advantage #11: “Fewer dietary restrictions and demands on the mother”.
Perhaps this means formula feeding mothers have worse diets because they don’t feel they need to eat healthily. Point: everyone should eat healthy, breastfeeding or not.
- Advantage #12: “It is safe for you to take antibiotics or other medication as these will not transfer into your baby through your milk”.
Most medications are safe to use whilst breastfeeding, and for those that aren’t, there is almost always an alternative to switch to.
- Advantage #13: “No interference from sore or leaking breasts when resuming sexual relations”.
Sure, if your bedsheets are more important than your baby’s nutrition...
Well that’s the entirety of Alison’s list of formula feeding pros. Notice that Alison gives 7 advantages to exclusive breastfeeding and 13 advantages to exclusive formula feeding! Alison swiftly follows this biased collection of lists with the following paragraph, which I read half-way then balked:
“Every woman’s breastfeeding experience will be different from the next and while some will cope with ease, others will never feel comfortable with breastfeeding and won’t particularly enjoy it. There is a very good book by Clare Byam-Cook called...”Nooooooooooo! (imagine me leaping through the air in slow motion grabbing the book from your hands). This paragraph reads like the old boys’ network of breastfeeding saboteurs. Clare Byam-Cook has as much faith in your ability to produce sufficient breastmilk as I have in Charlie Sheen becoming the next Pope. Avoid! Clare Byam-Cook believes that the breasts of many mothers are innately broken (see
here). As Clare and Alison are on the same page when it comes to undermining breastfeeding, it is with fake shock that I balked at this recommendation. Alison describes Clare’s book, “What to Expect When Breastfeeding...And What If You Can’t?” as:
“in my view, the best and most comprehensive guide on the subject” (page 29).
Which roughly translates into – it’s a pile of crap, the pages of which shouldn’t even be used to wipe the ass of your ex husband.
It shouldn’t come as much of a surprise (not even enough to lift a gnat’s eyebrow) that Alison is very much against co-sleeping. This is because co-sleeping requires the parent to share their sleeping quarters with the inconvenient produce of their loins. This, as Alison tells us, is simply not conductive to the success of her sleep plan:
“When giving night feeds try to resist temptation to take your baby into bed with you to feed him. It is far better to sit in a chair and carry out the feed with minimum fuss” (page 104).
Minimum fuss? Dragging your ass out of bed, going into the other room, dragging your baby’s ass out of bed, then sitting on a chair, freezing your respective assess off as you sit upright for up to an hour - this does not seem like minimum fuss to me. Yet Alison persists:
“If you are breastfeeding you will have more success using my plan if you follow this advice rather than feeding your baby while lying in bed” (page 104).
Why single out breastfeeding mothers? Call me a cynic, but the focus on nursing mothers is a probably because co-sleeping perfectly lends itself to breastfeeding, thus making the whole feeding process more efficient, speedy and enjoyable; but facilitating breastfeeding is
not what Alison’s about. She continues:
“I also advise that very early on you begin to offer at least one of the night feeds from a bottle” (page 104).
“I advise using the bottle for the bedtime feed at 7pm. I have found this to work fairly well for a number of reasons:
•It can provide a busy working dad with the opportunity to have some contact and be involved with baby before bed” (page 105).
I’m going to sound like a Vtech product by repeating myself in monotone again and again but: there. are. other. ways. to. bond. with. a. baby.
•“After a long, tiring day, your breast milk supply may be diminishing and may not be enough to sustain your baby throughout the night” (page 105).A double whammy here. Firstly, Alison dissuades nursing mothers from giving their breasts the stimulation they need during the evening – when they need it most. Secondly, she tugs on the nerve in every nursing mother’s brain that worries whether she is producing enough.
•“Babies are also very often tired after a long day and may not have enough energy to take a full feed from the breast” (page 105).If you don’t bottle-feed for yourself, stop being selfish and bottle-feed for your baby! The poor soul is knackered. Makes you wonder how we aren’t an extinct species.
•“It is usually quicker to give a bottlefeed, therefore giving you more free time each evening” (page 105).I was wondering how long it would take to switch back to “babies are inconvenient” mode.
•
“It gives you an opportunity to see how much milk your baby has had and therefore to be confident that he should not require another feed till morning” (page 105).
...or freak you out if he has only taken 2oz.
If your baby still insists on feeding through the night, it’s time to step the deprivation up a gear. Alison instructs you to water down your baby’s bottle-feeds to trick the little blighter into disinterest:
“Q: My baby is eight weeks old and is still waking at around 3am and expecting a feed. What shall I do?
A: Some babies may need a little more training to do without the last feed completely. The contents of a bottle can be gradually diluted and the volume reduced to reduce your baby’s reliance on nourishment during the night. If you are feeding with expressed breast milk, it can be diluted by adding cooled boiled water, and if using formula you can begin to reduce the number of scoops you add to the usual amount of water” (page 104).
The book includes a chart instructing exactly how to dilute your baby’s feeds. If you’re exclusively breastfeeding, there’s a chart instructing you to reduce your baby’s time on the breast:
The advice is repeated on page 140:
“By 8 weeks old your baby should be showing signs that he really doesn't need a feed during the night. If he is still waking in the early hours and looking for his feed, this might be the time to think about watering it down”.It is just as dangerous to dilute your baby’s feed too much as it is to make it too concentrated. Too little powder will reduce the baby’s ability to gain weight properly and make him hungry. It also makes the formula even more nutritionally imbalanced. Furthermore, if done regularly, diluting formula puts the baby at risk of water intoxication (overdosing on water is difficult to do as a child or adult, but actually relatively easy for a baby), fluoride overdose (most tap water contains fluoride) and sodium overdose (some tap water contains high levels of sodium and babies are particularly sensitive to its effects).
So, once your baby starts sleeping through, thus dropping that night feed, presumably that means the breastfeeding mother can stop using the bottle? Not on your nelly!
“When your baby is sleeping through the night without requiring a night feed, chose one of the daytime feeds to replace with the bottle, thus keeping at least one bottlefeed in place during each day to ensure your baby’s prolonged acceptance. It is entirely up to you which feed you chose” (page 105).
So I’ve left my newborn to cry for hours, deprived him of comfort when he’s upset, forced him to take a bottle, and starved him through the night. How else can I bully my baby into subservience?
Well once you’ve starved your baby through the night, it’s time to get cracking on starving him through the daytime. He’ll be wanting your attention then too, and we can’t be having that:
“After around eight weeks your baby should have responded well to the plan, be sleeping through the night and no longer needing a night feed. Once he has consistently slept through for around 12 hours each night for at least two weeks, you can gradually start to reduce the number of daytime feeds” (page 115).
Okay reduce daytime feeds – check. I think my baby’s spirit is almost broken, but I want to make doubly sure. How do I accomplish this?
![]() |
| From page 178. |
“Whatever sleep aid your baby has been used to settling with will now be removed and you will put him into his cot, say your goodnight phrase, leave the room and close the door behind you. More likely your baby will start to cry and may even be at full pitch before you can get through the door, but summon all your resolve, ignore him, carry on out of the door and close it behind you” (page 172).
I can’t leave my baby to cry, can I? What if he’s ill, or hurt?
“If you allow your baby to use his cry as a method of drawing you in, it will end up with your baby dictating his own terms and being in control instead of you!” (page 193).
Neglecting an 8 week old to the point where they cry themselves to sleep (sans blankie or whatever shred of comfort they have left) is one thing, but what about a 12 month old – those little sods are mobile! To address this dilemma, Alison suggests physically restraining your 12 month old into submission:
“Your baby will be more mobile and will be able to stand up in his cot, so you will need to put him back down firmly into his sleep position” (page 183).
Alison then describes a scene she observed via video camera, in which she believes
proves that babies are tyrants:
“I have witnessed many babies of this age group [12 months] via a video camera that I put in their room during the sleep-training process and it is fascinating to see how their reactions change as the training progresses. To start with they may be continually standing up and even shaking the bars of the cot with utter frustration, shouting at the tops of their voices, but after a while they run out of steam and can only manage a sitting position, from which they eventually give up and lie down to sleep” (page 183).
This scene can be described in many ways, heart braking and desperate for sure, ‘fascinating’ it is not. I’ve never burnt a book in my life (and I’m a law graduate, so believe me, I’ve come close), but this book has taken a steaming dump on my love of literacy. It is only deserving of lining my cat’s litter tray. Alison’s ‘work’ is yet another variation on the tired old theme: “Just let them cry it out”. This tough love for babies is like training a pet. Babies like the video-taped one described may eventually give up crying and go to sleep, but they lose their trust in their parents to meet their nighttime needs. They disengage from external stimuli and retreat to a lonely internal world.
And with that thought, I condemn this book to ash.
The Ultimate Baby and Toddler Q&A Hollie Smith 2012
Ahhhh Netmums, the cosy nemesis to Mumsnet (only not as articulated nor as widely quoted in newspapers). This book attempts to be a massive collection of questions and answers covering a comprehensive range of baby and toddler topics. There is some genuinely sound advice in parts; the book is big on skin to skin for example, and it recommends La Leche League. However other parts are utter tripe. Ironically, it is because the book contains an uneasy mix of good and bad advice that makes it even more insidious. The good tends to mask the bad, which sets a perfect trap for unsuspecting parents.
Our first introduction to breastfeeding is in a chapter titled, “Is breastfeeding supposed to be this difficult?” Here we find the inaccuracies begin:
“If you’ve hit a rough patch but you’re determined to feed your baby for the optimum six months that’s officially recommended, or beyond, then your best bet is to seek as much help as you can in finding a solution, and battle on” (page 55).
![]() |
| Page 55. |
Six months is certainly not the optimum length of time for breastfeeding, and no medical organisation (Government or otherwise) suggests this. The 6 month assumption plays into the myth that, there’s no nutritional value to breastfeeding after 6 months. The sentence should read: “feed your baby
exclusively for six months,
and then continue until your child is the optimum age of 2, or beyond, as recommended”. If the book is going to cite ‘recommendations’, it can at least state the facts correctly. There is, after all, a massive difference between 6 months and two years.
The book continues, predictably, by covering the well-chartered topic of guilt:
“If, on the other hand, difficulties with breastfeeding are making you truly miserable; or are causing problems for other members of the family; you should certainly consider alternatives. Either way, it’s not something you need to feel guilty about” (page 55).
If you’re going to give up breastfeeding because other members of the family have beef about it, then you, my friend, are a pussy; and guilt seems quite an appropriate emotional response in the circumstances.
“As a health visitor I absolutely support breastfeeding, but not at the expense of what’s best for those involved; and bottle-feeding with love is just as good” (page 56).
Ahhhh I knew I should have suspected one of those weasels sniffing about.
Never trust a health visitor. At least not until you’ve sought several second opinions. Let’s quickly tackle this sentence in its component parts:
“As a health visitor I absolutely support breastfeeding...”Firstly, being a health visitor does not necessarily equate with supporting breastfeeding. Secondly this is a classic introduction to a sentence which is about to undermine breastfeeding. It’s like Hugh Hefner saying, “I’m not a dirty old perv but...”
“...but not at the expense of what’s best for those involved;”The two main players here – the mother and the baby – each have interests on the line. Breastfeeding is certainly best for both of these parties - biologically speaking. However when the nutritional interests of the baby collide with the practical interests of the mother, it makes logical sense that, life-threatening scenarios aside, the baby’s interests should trump the mother’s. The baby is the person whose voice is the quietest both literally and metaphorically and who has the least control over the situation. Not to mention the moral and practical fact that the parent produced the child, and is thus responsible for safeguarding it’s welfare (bizarrely this appears to be a radical concept in modern society).
“bottle-feeding with love is just as good” (page 56).
Bottle-feeding is not ‘just as good’, whether ‘with love’ or otherwise. Even formula companies publicly recognise this. Furthermore, even if the bottle contains expressed breast milk, some of the protective effects of direct nursing are lost.
Next, the book elaborates:
“It’s not just about what’s best for your baby, it’s about what’s best for you and your mental health. You may also need to take into account your partner’s feelings and the needs of the rest of your family” (page 58).
Again, I remind you that the baby has no voice. If his own mother isn’t going to safeguard his best interests, then who is? Consider also, whose interest is most fundamental - the mother’s desire for comfort and convenience or the baby’s need to be protected from lifelong health risks? Arguably, the mother’s desire for comfort and convenience is a ‘secondary interest’ and the baby’s need to be protected from lifelong health risks is a ‘primary interest’. It stands to reason that a secondary interest should be sacrificed to promote a primary interest. Yes, that means a certain element of martyrhood, but what are parents if not martyrs in some respect?
Needless to say, the book’s perspective on breastfeeding is pessimistic and defeatist:
“If you decide to drop breastfeeding, you should do so without regret. The ‘breast is best’ lobby is a powerful one. While for some women breastfeeding can be an empowering and life-enriching experience, for others the physical, emotional or social challenges can seem less of a dream and more of a nightmare” (page 59).
Here’s a secret – you don’t have to enjoy it. We parents have to endure many things we don’t necessarily enjoy: sleepless nights, early mornings, dirty diapers, toddler tantrums, Build A Bear parties, the list is endless. Man up.
And while you’re at it, stop perpetuating propaganda such as this tired old cliché:
“At the end of the day, we all want what’s best for our kids, and the best gift any baby can receive is a contented mum” (page 59).
This parent-centric stance is simplistic, not to mention egotistical and narrow-minded. What a baby would regard as ‘the best gift’ is entirely subjective (due to babies having no voice as I mentioned earlier), and subjectivism has little place in important medical issues. I’ll say it again, ‘happy mom – happy baby’ is simplistic, egotistical and narrow-minded. Right on cue, a mother matching this description chimes in with her experience:
“Breastfeeding was a nightmare for me. I was scared to suggest bottle-feeding, as the midwives seemed dismissive of it. Finally, one suggested a combination of breast, expressing and formula, but it made me feel my whole life revolved around feeding! After six weeks, we went fully on to formula. Finally, I knew my baby was getting the food she needed – Jenny from Stockport, mum to Laila, two” (page 59).
Another mother from the simplistic, egotistical and narrow-minded club shares her experience:
“My whole life revolved around expressing and I felt like a cow. Looking back, I wish I’d given him formula sooner. – Irma from Oldham, mum to Damir, four, and Aydin, two” (page 62).
And another:
“At three months, for some reason, my son stopped wanting any breast and switched permanently to the bottle. I felt very un-needed. However, he’s now a very healthy little man of ten months. I believe it doesn’t matter whether your baby breastfeeds or bottle-feeds – as long as he feeds. – Anne-Marie from Royston, mum to Thomas, ten months” (page 63).
Notice how she blames her son for switching to the bottle, like he leapt out of his crib one day and decided to boil the kettle and prepare his own formula. It appears blaming the baby is commonplace. Here’s another mother doing so:
“Thankfully, she went for the bottle straight away, no problems. At six months she switched herself exclusively to bottles, mainly all formula by then. – Anna from Newton Abbot, mum to Issac, three, and Milly, two” (page 139).
So she made all the bottles up herself did she?
Then, for good measure, there’s yet
another tale of woe:
“I breastfed for a few months then got hospitalised with mastitis and found feeding from then on very stressful, so finally moved to formula. Jessica is certainly none the worse for it. – Debbie from Croespenmaen, mum to Jessica, five, and Ethan, two months” (page 60).
And another FFS!
“I made a good start with breastfeeding but by day four I wasn’t producing enough milk and so I swapped to bottles and formula. With an older child and a toddler too, it’s been more practical for me to formula feed. I’m glad I gave it a shot, though. – Nicola from Bournemouth, mum to Toby, six, Anise, sixteen months, and Lukas, three months” (page 60).
What this mother doesn’t say, is how she knew she was producing insufficient milk. Consequently, this tale is of no help to anyone, yet perpetuates the ubiquitous myth that a significant amount of women have ‘broken boobs’.
And, just in case you didn’t notice a theme developing, here’s another tale of breastfeeding woe:
“I was basically a milk cow: express for thirty minutes, feed for thirty minutes, wash up and steralise everything, twenty minutes for a wee and a cuppa, then start all over again. At six months, my daughter got a snotty cold and decided bottles were easier. A happy, relaxed mum is more important than the method of milk delivery. If you need to stop breastfeeding due to pain/stress/sanity, then do. – Anna from Newton Abbot, mum to Isaac, three, and Milly, two” (page 60).
Looks like this mother has fallen into the common trap of downplaying the importance of breastfeeding in order to make herself feel better for quitting. Contrary to what she spouts, breastfeeding is much, much more than merely a ‘method of delivery’, as any exclusively pumping mother will tell you. By dismissing the qualities of breastfeeding, this mother, (and all those who apply this strategy), are undermining breastfeeding mothers who battle on in the face of adversity. After all, if breastfeeding were simply a ‘method of delivery’ how foolish it would be to battle through stress, mastitis, cluster feeds, thrush et al when apparently bottle-feeding is just as good. It makes breastfeeding mothers look like quacks.
The book continues to present an imbalanced collection of breastfeeding stories, tipping the scales with yet another tale of woe:
“Jake was my first baby and I intended to breastfeed. Unfortunately, I wasn’t shown how to feed him correctly and he didn’t latch on right. I kept trying, but Jake kept screaming, so we gave formula and he became a calm, contented baby. – Rachel from Staines, mum to Jake, five, Kyla, four, and Abigail, five months” (page 61).
Here’s an idea, how about seeking help rather than waiting for it to come to you? How about doing some research before giving birth? Finding your local breastfeeding group? Phoning a helpline?
This mother didn’t bother to tap into any of these support sources, and this book doesn’t bother to mention them. Instead, it prefers to print tale after tale of woe with no indication that these problems can be resolved. Here’s a curiously vague tale:
“With my daughter, it took four days and a lot of tears from both me and her before the midwife realised I wasn’t producing anything at all” (page 62).
So the mother switched to formula at 4 days... when her milk was due to come in. Imagine, if you will, Homer Simpson proclaiming: "Doh!" But the book doesn’t mention this important biological fact. The mother then adds:
“A fed baby is a happy baby” (page 62).
Imagine Nelson's "haaa-haaaa!" at this point. A fed baby is a happy baby, where do they get this crap? Sounds like text lifted straight from a Cow & Gate can, then regurgitated by deluded mothers the world over. A fed baby is not necessarily a happy baby, particularly when they have colic, an ear infection and reflux caused by consuming formula; oh and
especially when they’re dead from SIDS. Just sayin'.
Another case of lazyitis can be found later on page 85:
“My son just would not suck, and I ended up bottle-feeding with formula from day two. I did give expressing a try when my milk came, but it just took too long. – Emma from Banbury, mum to Nathaniel, four months” (page 85).
One thing that pokes you in the eye like a 10 month old’s finger, is the blatantly imbalanced portrayals of breastfeeding experience in this book. It is so obviously tipped in favour of giving up. This defeatist attitude pretty much continues throughout the entire book.
Take the next example for instance, it demonstrates how mothers often declare they ‘had no choice’ when in fact, they couldn’t be bothered to pursue other options; In the chapter titled, “Is it OK to give him a dummy?” one mother declares:
“Breastfeeding was so painful, there’s no way I was going to let him comfort suck on me. So we had no choice but to try a dummy. I was worried that he’d develop nipple confusion but he never had a problem switching between the two. – Helena from York, mum to William, six months” (page 75).
To shun the risk of nipple confusion further:
“I gave Isabella a dummy as she needed the extra comfort. She still has it now, but she’s also still breastfed, so it hasn’t caused any problems there. People can be really snobbish about dummies. They carry a real stigma for some reason – I suppose there’s the suggestion that you should be doing more to comfort your child. – Leanne from Bath, mum to Isabella, fourteen months” (page 75).
Who would suggest such a thing? *chortle*
![]() |
| Page 77. |
Predictably, yet more tales of woe abound in the chapter titled, “How do I know I’m feeding her enough?”:
“I breastfed my eldest daughter and she seemed to want to feed constantly. By week nine I’d had enough. I didn’t feel it was worth it because I couldn’t be the mummy I wanted to be, as all I was doing was sleeping or feeding. So I gradually weaned her off me and on to the bottle. It was the best decision I made as my energy came back and I could begin enjoying my baby. I weaned my second baby on the bottle at ten weeks too. – Stephanie from Rochdale, mum to Emily, four, and Lily, two” (page 82).
It’s all about
you isn’t it?
Tales of woe such as these create a culture of failure which serves three purposes. For pregnant mothers who have not decided how they will feed, it turns them off the idea of breastfeeding. For breastfeeding mothers, the carefree dismissal of breastfeeding undermines their efforts. And for formula feeding mothers, it plays into their denial and soothes their guilt. In other words, stories like these serve no positive purpose.
Furthermore, what is left
unsaid is as important as what is said. Take this tale of woe for example:
“I’m too scared to try just breastfeeding on its own as I don’t think I have enough milk. – Helen from Bristol, mum to Max, six weeks” (page 82).
The book makes no effort to reassure readers that it is highly unlikely they will not have sufficient milk. It just leaves the fear hanging in the air like that stale fart I spoke of earlier.
![]() |
A: When hell freezes over!
Muhahahaha! |
Up to this point, the book has established itself as parent-centric, aiming to appeal to those parents wanting maximum convenience at minimum effort with baby’s needs as an afterthought. This theme continues into the sleep chapter titled, “When will he sleep through?”:
“It’s a good idea to start encouraging your baby to self-settle as early as possible, because what you’re aiming for is for him to get himself back to sleep when he wakes in the night, rather than waking you and demanding your services” (page 129).
So the book champions ‘self-settling’ on one hand, yet on the other hand advocates using formula to feed your baby to sleep:
“Lots of breastfeeding mums wonder if a bottle of formula given last thing at night will help. It’s true that formula isn’t digested as easily as breast milk and is likely to leave a baby feeling fuller for longer. If you’re truly exhausted, it may be worth trying” (page 129).
What new parent isn’t ‘truly exhausted’? Still, it would seem that bottles are the answer to everything:
“I think it’s a good idea for all babies – even those that are exclusively breastfed – to be happy about taking a bottle. For that reason, I’ve always advised breastfeeding mums to offer supplementary drinks of water in a bottle from quite an early stage” (page 136).
Apparently, this is an ‘expert’ talking. God help us all. She continues:
“Mixing bottle and breastfeeding can work very well, in spite of the common view that it’s a ‘slippery slope’ that will soon bring about a complete end to breastfeeding. Just be aware that introducing a bottle can be harder the longer you put it off” (page 136).
But what if your baby won’t take the bottle, because understandably, he prefers a warm, soft breast with a human attached. In that case, the book suggests
starving your baby into submission:
“There’s always the ‘cold turkey’ approach based on the theory that your baby will have to accept a bottle if she becomes hungry enough. Be warned though, they can hold out for a long time: you may find that your nerves desert you” (page 137).
...and damage your baby’s trust in your ability to fulfil his basic needs, whilst you develop mastitis or a breast abscess. Nice.
But why is it so important to introduce a bottle, even if you are exclusively breastfeeding? Answer: So Daddy can bond with baby of course! Duuuuh! If Daddy is denied the opportunity to place a plastic teat in his baby’s mouth, he may get resentful, your marriage will fall apart and he will run away with the Wallmart checkout lady. Or something:
“I’ve been trying to get my baby to move to bottles for a few weeks now but she’s so stubborn – she just doesn’t want to know. I end up giving in and feeding her myself. My husband is desperate to feed her himself. I think he feels he’s reliant on me always having to take over and it’s getting in the way of their bonding. He does do everything else he can – baths, massage and play, but that feed before bed is such a special time and I wish he could get some of that. We’ve taken a break over the last week as she was getting very worked up and we are hoping to have another go next week. – Sarah from Darlington, mum to Jack, three, and Beth, four months” (page 138).
This baby clearly doesn’t want the bottle, yet her parents are ignoring her wishes because of some warped view that a bottle is necessary to paternal bonding. In the book I wrote a big “Oh FFS!” next to this (and as a rebel, I shall return it to the library like that).
Another example of a parent resenting their baby’s natural preference can be found on the next page (I know what you’re thinking - this book sure is balanced!):
“My son was no problem and would go from boob to bottle and breast milk to formula with no fuss. With my daughter it’s been a different story as she would not take a bottle or formula, which meant having to carry on breastfeeding far longer than I really wanted to! I am pro-breastfeeding but think that new mums should be advised to give a baby a bottle-feed regularly and fairly early on so they get used to it. – Michelle from Hitchin, mum to Ed, two, and Evie, eleven months” (page 139).
Michelle, despite your claim to the contrary, you’re clearly not ‘pro-breastfeeding’ as if you were, you wouldn’t want potentially sabotaging advice pushed onto new mothers. Speaking of which, let’s move on to the chapter about weaning.
![]() |
| Page 182. |
Weaning, in this book, refers to the UK interpretation of the word, meaning ‘introducing solids’. The chapter begins:
“If you have a big baby who no longer seems content with just milk feeds, or has taken to waking up in the night where she’s previously been sleeping through, or is sitting on your lap at mealtimes and trying to take stuff off your plate, then maybe it’s time to consider weaning – even if she isn’t yet six months old” (page 183).
Let’s go through each of the book’s signals to weaning readiness, and look at what the causes are:
“baby no longer seems content with just milk feeds”Cause: growth spurt.
“waking up in the night where she’s previously been sleeping through”Cause: growth spurt.
“sitting on your lap at mealtimes and trying to take stuff off your plate”Cause: being a baby.
None of the above require you to introduce solids to your baby shy of the World Health Organisation guideline of 6 months. Yet according to this book, the WHO don’t know shit:
“There’s no clear evidence that introducing solid food somewhere between four and six months – as opposed to waiting for six months – could be harmful” (page 184).
With hundreds of studies about gut readiness under their belts, good parents tend to err on the side of caution. Waiting until 6 months to introduce solids will not damage your baby, however introducing solids prematurely is certainly linked with health damage. Why are some parents impatient at introducing solids? Why are they willing to risk their baby’s health? Answer: because they (foolishly) believe that introducing solids will make their baby sleep more/cry less and otherwise be less demanding. This is the lazyitis epidemic again. Books like this one, know what such parents want to hear, and are more than willing to supply it. ‘Give formula, it’s fine. Give solids early, it’s fine. Really. There’s no need to feel guilty.’ This dangerous writing puts a smile on parents' faces and dollars in the authors' pockets but the casualties are the babies. Case in point:
“Even these high-risk infants are no better off if their exposure to potential allergens is delayed until after six months, rather than if you make a start somewhere between four and six months” (page 185).
Basically, the book is harking back to the 1980s age of weaning, and in the process, pissing on thirty years of scientific research.
“Don’t assume if you breastfeed and/or delay weaning that it will definitely protect against allergies developing” (page 185).
Well DUH! Not smoking doesn’t guarantee that you won’t die of lung cancer, but it’s a bloody good place to start!
![]() |
| Page 216. |
Staying with the lazy angle, the book has a chapter titled, “Is it OK to start sleep training?” Geeee can you guess what the answer is? A big fat
hell yeah:
“Rather than giving him that feed, or whatever else he’s looking for when he wakes in the night, or when you put him down for the evening and he won’t settle, you make sure he knows it is not available – and that he needs to go to sleep, instead. And as a general rule, the sooner you try it the easier it’s likely to be” (page 217).
No age limit is given. If fact, parents are advised to night train as soon as possible, which can be dangerous for young babies or babies that are unwell. Speaking of being a danger to babies, Dorothy Einon, the author of the next book we are going to look at, comes pretty high on the list...
Dorothy Einon’s Complete Book of Childcare and DevelopmentDorothy Einon 2004
Somebody’s been taking back-handers from formula companies. Or so you’d think if you read this book. The book begins, naturally, with the topic of birth, which is a perfect opportunity for the author to say:
“The odd bottle of formula is not the end of the world (or of breastfeeding)” (page 13).
What an optimistic start to the book. At least we know from the outset where the book stands on the issue of exclusive breastfeeding (i.e. it’s unimportant).
Indeed, breastfeeding itself, is belittled:
“Breasts are a convenient means of delivering food. They do not deliver love” (page 13).
This statement is factually inaccurate on a physiological and also pragmatic level. Oxytocin, the hormonal of love, is delivered through breastmilk. Therefore love is, in fact, delivered through breastfeeding. Furthermore, breastfeeding, unlike formula feeding, is more than merely ‘a means of delivering food’. Aside from the hormonal transaction between mother and child, breastfeeding is also a means of delivering immunological support, optimum nutrition, and also provides nature’s protective measure against ear infections and jaw misalignment (the auction of suckling at the breast facilitates oral development which has a positive knock-on effect for speech development!) Phew.
![]() |
Page 20.
Notice the bold caption 'Better health?' |
None of these attributes are mentioned in the “Breast or bottle?” chapter, which tilts in favour of bottle feeding. The introduction to the chapter reads:
“Always remember: a breast is just a breast. How you deliver milk to your baby is a very minor part of parenthood” (page 20).
Actually, feeding is central to babyhood. It is a baby’s prime source of pleasure and comfort, and essential for their growth. Indisputably, it is central to your baby’s ability to thrive; they spend most of their time doing it, and it is central to their survival and well-being. Therefore if you have a baby, feeding is not only a major part of parenthood, arguably it is
the most important part of parenting an infant. Start as you mean to go on people.
The text continues:
“If you cannot breastfeed your baby, for whatever reason, this should not make you depressed. No-one ever tells you that you should not breastfeed, but the advantages of breastfeeding are often overstated. Here we will look at some of the claims in detail” (page 20).
Oh goodie. Lets.
“Breast milk is designed for rearing human babies, cow’s milk for rearing calves’, goes the argument. Formula is cows’ milk that has been modified to make it more like human milk. It is not perfect, but fairly good – if bottles are made up as directed, formula provides your baby with all the nutrients she needs to grow. It does not change throughout the feed, as breast milk does, not does it adjust as the child grows, but whether this is necessary is not certain” (page 20).
So the author claims that formula is ‘fairly good’ at mimicking breast milk (Fact: it’s not; see
here). Even if this were true, what parent would choose ‘fairly good’ for their infant’s nutrition? Not good, just ‘fairly good’. If you’re willing to downgrade to ‘fairly good’ for your baby’s nutrition, what other areas of parenting are you willing to cut corners on? Nappy changing perhaps?
“Babies are happy in wet nappies” (page 13).
Soooo anyway, back to the analysis of breastfeeding health claims:
“There is less sodium in breast milk – while this is better for the kidneys, bottlefed babies are no more likely to suffer from kidney disease” (page 20).
Breastmilk has a low renal solute. Renal solute load represents the amount of waste products excreted by the kidneys, per liter of milk consumed. The major determinants of renal solute load are dietary protein and electrolytes such as sodium, potassium and chloride. Breastmilk has a low renal solute load compared to formula. In non-nerd language this basically means by breastfeeding your baby there is less work for his developing kidneys, compared to the load if he was formula fed. Yet Dorothy seems to think that putting a baby’s kidney’s under strain is all fine and dandy.
“Breastfeeding is claimed to protect against gastroenteritis, cot death and cancer, and to promote better cholesterol metabolism and intelligence. This is difficult to prove or disprove because, in most cases, studies do not compare like with like. Mothers who bottlefeed are more likely to be poor, to live in substandard housing, to be teenagers, smokers, drinkers, drug takers, and to have fewer years of education. On average their children are more likely to suffer from disease, but whether this is a direct result of being fed by the bottle rather than the breast or because of other reasons is unclear” (page 21).
Most major studies account for these variables and still show formula feeding to be substandard. Next!
“We cannot even say for certain that the immunity comes directly from the breast milk. The immunity breast milk passes on to the baby would far outweigh all the advantages of bottle-feeding if we lived in a less sterile environment. However, today bottle-feeding is completely safe as our modern homes are clean of germs. When our immunity is rarely challenged by attack, the advantages of breast over bottle become less obvious” (page 21).
When babies are born their immune systems are very immature; this means they are susceptible to many different illnesses and allergies
regardless of how sterile their environment is. Breast milk contains a variety of immunological, antimicrobial and anti-inflammatory agents that protect against infection. Approximately 80% of the cells in breast milk are microphages, cells that kill bacteria, fungi and viruses. Furthermore, the pH balance of breastmilk differs to that of infant formula. The pH of breastmilk aids the growth of friendly microbes (probiotics), specifically lactobacilus bifidus, which prevent the growth of more harmful organisms (see, '
The Virgin Gut: A Note for Parents'). Also, unlike formula, breast milk is sterile (it has no germs). It does not need to be stored and it does not become contaminated by polluted water or dirty bottles, which can lead to infant diarrhea.
The next issue the author wants to tackle on her whistle-stop tour of breastfeeding health claims is – the topic that presses the tetchy button of many formula feeders – bonding!
![]() |
| From page 21. |
“It is true that bottle-feeding can be carried out by others, or that by propping the bottle on a cushion you can feed a baby without even picking her up. But that does not mean that mothers do not bond as they bottle-feed. Breastfeeding mothers do not always gaze lovingly into their baby’s eyes as she suckles. For many of them breastfeeding is a time to catch up on reading or talking to an older child. While it is hard to change a nappy, or spoon feed, or jiggle a bottle teat into the mouth while having a conversation, it is perfectly possible to slip the nipple in the mouth while doing so. There is no evidence that the breast is the seat of love, and we can safely ignore all claims that it is” (page 21).
I’ve got no idea what “the seat of love” rhetoric actually means. More importantly, this paragraph fails to mention the hormonal exchange between mother and child which occurs during nursing, nor the codependence of nursing mother and her child, nor the inevitable skin to skin contact of breastfeeding; all of which contribute to the enhanced bonding experience that the breastfeeding dyad enjoys above the formula feeding dyad.
The book even alludes to the fact that breastfeeding mothers enjoy enhanced bonds with their babies (the book refers to this as ‘closer emotional ties’), yet of course, shrouds this in negativity:
“While mothers may develop closer emotional ties to their breastfed babies, fathers may lose out. They may feel less excluded from this close relationship in the early weeks if the baby is given at least an occasional bottle” (page 21).
This assumes that the bond a mother develops with her breastfed baby acts to the detriment of the father. It suggests that the baby only has so much love to go around, and the breastfeeding mother has swiped it all for herself. Nonsense. Fathers are not Oliver Twists, with quivering bottom lip and cap in hand, pleading, “can I have some more (love) please”. And if your husband is like this, do consider an exchange.
![]() |
| From page 24. |
However, like an offended mother on Facebook, the author won’t drop the issue. Many pages later, she’s still talking about poor daddies:
“Most surveys suggest that mothers still do far more of the day-to-day caring for the children than fathers. Part of the problem arises because men cannot breastfeed a baby. Most babies are comforted by the breast, and because men do not have this ‘comfort object’ they are less able to quieten crying babies” (page 139).
Did you hear that ladies, your bloke is incompetent because you breastfeed! It doesn’t occur to him to cuddle, rock, or talk to the baby.
Like the other books featured in this article, this one sticks to the patronising approach of giving formula feeding parents ‘permission’ not to feel guilty:
“Never feel guilty about giving your baby a bottle. Regard the bottle as a liberating tool” (page 46).
Why would a formula feeding parent feel ‘guilty’? Answer: Because they’ve put their own wants above their baby’s needs. Telling parents to regard bottles as a ‘liberating tool’ simply feeds this selfish rhetoric.
![]() |
| From page 46. |
The book then awkwardly attempts to readdress the focus by suggesting that feeding is not an important part of parenting:
“Never feel that you have failed if you need to introduce a bottle. Parenting has very little to do with feeding the baby’s body, and everything to do with feeding the child’s mind, social development and his long-term emotional stability” (page 46).
...all of which are linked to his health, which is directly linked to his nutrition. As I mentioned above, a baby spends most of its time feeding and sleeping. If you fuck up at one of these, you’ve fucked up at 50% of parenting a baby, and no, you don’t get a rosette for that.
Thus far, all evidence suggests that this book doesn’t hold breastfeeding in high esteem. So at this point, any wise mother would close the book and seek breastfeeding support elsewhere. However if you want your breastfeeding journey sabotaged, the next chapter, “How to breast-feed” delivers the goods. So-called ‘expert’ advice includes:
“Introduce more, shorter feeds” (page 22).
“Start by giving 5-10 minutes on each breast” (page 23).
...and deprive your baby of the rich hindmilk he needs to thrive. In reality, you should let your baby decide how long he wants to feed on each breast. If he’s taking his sweet time and you’re impatient, you can check he’s still feeding by looking for cues such as rhythmic sucking and swallowing, baby’s cheeks staying rounded when sucking, and wiggling ears.
More twaddle passed off as fact includes:
“What you drink, he drinks” (page 23).
No Sherlock. When you down a shot of vodka, baby is not downing the equivalent. Very little alcohol enters breast milk.
“Supply might be low at night so you may need to supplement with formula” (page 25).
Babies tend to be fussier at night (over-stimulation and tiredness mostly), consequently many mothers falsely believe their baby is fussy because they are not receiving sufficient milk, which leads the mother (as per the instructions in this book) to supplement with formula, which results in their supply
truly diminishing. Thus, inaccurate information such as this becomes a self-fulfilling prophecy.
“It’s easier to wean your baby off the breast before his first birthday” (page 46).
What use is this info? It implies that all mothers should wean their babies shy of World Health Organisation guidelines so they don’t end up with teens forcefully latching themselves onto the breast.
Also in the “How to breast-feed” chapter, there’s a list of reasons “when not to breast-feed”. It’s like a list of excuses for the uncommitted mother looking for a get-out clause. The list includes such myths as:
“Don’t breastfeed if you have a serious illness, such as heart of kidney disease, or a serious infection, such as HIV/AIDS or TB” (page 23).
“Don’t breastfeed if you are seriously underweight” (page 23).
“Breastfeeding mothers may be more susceptible to depression. You may wish to take this into account if you are prone to serious depression and/or have previously suffered from postnatal depression” (page 23).
This last point on the list is particularly ironic. In fact, Formula feeding makes a woman more prone to depression than her breastfeeding peers. This is partly due to the fact that formula feeding mothers miss out on those loved-up breastfeeding hormones as well as the relaxation that said hormones provide. Breastfeeding is a biological imperative. By not breastfeeding, a woman is sending her body the message that her baby has died. Is it any wonder that hormone levels crash and depression is more likely (
Ystrom 2012).
The fact that a formula feeding mother is at greater risk of developing depression is omitted from the next chapter titled “How to bottle-feed”, along with a lot of other important facts. It seems, when deciding how to feed babies, the author of this book does not want mothers to make an informed choice. The bottle-feeding chapter begins in very large font:
“Bottle-fed babies are happy and healthy, as are their parents. Bottle-feeding is essential if you need to return to work early, and it provides a unique opportunity for mother and father to share the feeding of their child” (page 24).
This bizarrely random intro is a contradiction in terms. Take the first sentence for example, “Bottle-fed babies are happy and healthy, as are their parents”. This is the opposite of what she said earlier in the book:
“In practice bottle-fed babies tend to be more susceptible to colic, wind, and being sick” (page 20).
So the accuracy changes from page to page!
Re: “Bottle-feeding is essential if you need to return to work early”, this is obviously a false exaggeration; bearing in mind that, throughout the book, the term ‘bottle-feeding’ is used to mean ‘formula feeding’. There is no need for employed mothers to formula feed, instead, they can pump at various points during their working day or use donor milk.
More inaccuracies are littered throughout the book. The ‘Sleep’ chapter is a prime example:
“Some babies sleep through the night by the time they are one month old” (page 36).
Yeah, sick, lethargic babies.
What if your (perfectly normal) baby doesn’t sleep through by this deadline? You can guess what’s coming!
“If he thinks by crying he can get you back to sit with him and stroke his hair why would he fail to cry? If he always goes to bed unwillingly he is best ignored. Check once and leave. If he carries on protesting, you have a choice. You can tough it out now, or live by his demands. His protests will fade, he will probably – reluctantly – accept the situation a few days later, and be firmly settled into the regime by the end of next week. Until then use earplugs, play some music, close all the doors, be firm and say “No, no and no!” – as often as necessary” (page 59).
This author has as much compassion and sensitivity as Simon Cowel's shrunken trousers. Rather than equip parents with the tools to
help their babies to sleep, she parrots the tired old Cry It Out regime. CIO by the way, is just another way of saying, ‘ignore your baby’. Parents who swear by this technique stick their head in the sand and go la, la, la, I’m not listening!’ (or use earplugs).
The ‘Establishing a Routine’ chapter is similarly misguided:
“Babies are flexible. You can mould them. There is no point in giving in to every feeding demand if this causes you to resent that you never have a moment to yourself” (page 40).
I highlighted the importance of demand feeding above. Suffice to say that if a mother resents her baby’s feeding cues, she’s going to have a tough time with toddlerhood, tweenhood and the teenage years. ‘Having a moment to yourself’ is a luxury of the childless.
But fear not; by Week 5:
“your baby should be starting to sleep through into the early hours before waking for his one and only night feed” (page 133).
I don’t know many babies who’ve received this memo. Perhaps the reason Dorothy believes babies should survive off only one single night feed at the tender age of 5 weeks is because she is passionate about making sure that babies get at least
some formula. Exclusive breastfeeding is therefore rejected:
“Statistics suggest that the majority of mothers give up breastfeeding around Week 7. Although there are many different reasons for this, I believe that it is in part due to the guidelines that suggest it is best for your baby if you exclusively breastfeed for six months. Rather than feeling under so much pressure, mothers should be encouraged to take a more relaxed approach to feeding. If they received support in introducing a supplementary feed as necessary – as my feeding guide suggests – I believe many would continue breastfeeding for longer. Surely if a baby receives at least some breast milk each day it is better than none at all? If you have reached this point and you want to give up breastfeeding, see Chapter 2, pages 49-54 for advice on how best to achieve this” (page 138).
So, according to Dorothy, in order to breastfeed for longer, mothers must introduce formula - despite the fact that formula supplementation has been
proven to decrease breastfeeding duration. The mind boggles. In fact, I have a sneaking suspicion that we're being fed gibberish. This suspicion carries on with this next book...
What Not to Expect When You’re ExpectingZoe WilliamsThe author Zoe Williams should be familiar if you are faithful to this blog. You may recall her previous work titled “Bring It On Baby” which I reviewed in
Part One. In fact, at the time of writing, it nabbed the coveted number one slot for most anti-breastfeeding book. Hurrah!
Well now Williams has written another ‘parentcraft’ book, and she has surpassed herself with this one: ‘What Not to Expect When You’re Expecting’. The title of this book is as plagiarised as its contents. In this work, Williams regurgitates most of her previous drivel, and unfortunately expands on it. Indeed, sizable chunks of it are lifted directly from her previous book. So let’s take a gander at her latest offering.
Williams has devoted a whole chapter to breastfeeding, titled: “Is Breast Best?” (woah inventive title! That sure as hell hasn’t been done before). Here, like before, she criticizes what she calls “the breastfeeding lobby”. She describes them as:
“inexplicably powerful: more powerful than the tobacco lobby” (page 82).
Yup, an invention of Williams’ imagination is apparently more powerful than billion dollar corporations. Even if we were to humour Williams and concede that a brestapo does exist (perhaps in the guise of public health messages touting the benefits of breastfeeding), there is no way such an organisation could ever trump the financial klout of industry. Yet Williams disagrees – and she has *proof*:
“Witness, in my lifetime, in my adult lifetime, it has become unacceptable to smoke in a pub, yet acceptable to breastfeed” (page 82).
Darn. I thought she might have attempted to come up with something more substantial. But no, she's suggesting that being in the vicinity of a breastfeeding mother is as abhorrent as being in the vicinity of people smoking. This deranged view of the world is echoed a few pages later with Williams' ‘slightly’ exaggerated description of breastfeeding in public:
“I ripped all my clothes off as if in a strip join frequented by early man” (page 85).
This scene, which occurs on a busy high-street, is the stuff of mediocre sitcoms, not of reality. Yet she proceeds to describe squiring herself in the eye with her own breastmilk, whilst standing in the street, as if it is a popular sport.
Another gem which is copy and pasted from her previous book involves Williams’ dismay at her inability to get what she deems a suitable, viewer-friendly photo of her baby nursing:
“If anyone can come up with a way to get a picture of a breastfeeding baby without getting a great big breast in the way, then I will find a way to give that person a Nobel prize” (page 86).
Here, Williams is confusing herself. The photo she actually wants to take is that of a baby sans breastfeeding. When a baby is breastfeeding, a breast is commonly part of the deal. Needless to say, Williams didn’t breastfeed for long:
“They were both weaned off breast milk by their half-birthdays” (page 88).
Fair enough. 6 months is still pretty good going. I have no beef with this. What I do have beef with however, is Williams’ excuses:
“One child had gone off breast milk, and would crane around the room looking for more interesting things” (page 88).
An inquisitive child does not a nursing strike make. Anyhoo, her other child apparently...
“wasn’t sleeping well, which I put down to the fact that breast milk only fills you up for about 36 minutes, indeed, from a sanitation perspective is useless, is essentially water that tastes of booze and garlic” (page 88).
Are you getting the feeling that Willaims’ doesn’t know much about breastfeeding, that she could do with reading ‘
Timeline of a Breastfed Baby’, that she needs a ruddy good bitchslap from the WHO? (The World Health Organisation, not the English rock band formed in 1964 by Roger Daltrey). The transparency of Williams’ vitriol towards breastfeeding becomes glaring when she declares Atlantic magazine’s much over-cited “
The Case Against Breastfeeding” to be a credible source (page 88). What then follows is one of the most pessimistic, defeatist views of breastfeeding ever to burn holes in my retina:
“For plenty of people, and I mean loads, I mean at least half of anybody I know who’s ever had a child, breastfeeding does not work that well. Some of them couldn’t get enough milk going, and actually never managed to; some had nipples that were too big, or a baby with a too-small mouth, or tongue-tie, or a baby that just didn’t feed, got jaundice from not feeding, had to go back to hospital and by the time it came out, was bottle-accomplished but no longer knew how to do it the old-fashioned way. Some had appendicitis and had to go into hospital when her baby was 14 days old, hadn’t had time to express; the baby was on formula for a week and then didn’t want to switch back (formula looks nicer; it would surprise me in no way if it didn’t also taste nicer). Some people get post-natal depression and had to stop breastfeeding to take Prozac, some other people got an infection in their c-section scar and had to take antibiotics that weren’t milk-friendly” (page 88-89).
This reads like a Defensive Formula Feeder’s bedside journal, rather than a childcare guide. At no point does Williams even hint at the fact that each of these obstacles - each and every one of them - can be overcome. Then she presents us with the most laughable excuse:
“Some other people were incredibly tired, and needed a break” (page 89).
Irony explosion!! So washing, steralising and preparing bottles gives tired mothers a break? Psyche! Yet the excuses keep coming:
![]() |
From the back cover
...seriously. |
“Some people just find it incredibly painful. One friend went to a breastfeeding workshop where a mother said it hurt so much, she was setting her alarm to go off 40 minutes before the baby woke up, just so she could neck enough analgesics and have time for them to take effect before she started” (page 89).
Great advice... if you want to appear on the government's Child Services register.
Williams’ negligent indifference to parenting penetrates into many other pages. For instance, she declares that she started giving one of her children solid food at four months:
“because I had a stringent friend and she told me to” (page 87)
...despite her appreciating that the recommendation was six months. She justifies her decision by framing it as a good one and belittling the scientific evidence:
“Paediatricians try to balance the protective qualities of breastmilk against the fact that four-month-old babies need more nutrients. They found that breastfeeding babies exclusively beyond four months was not stunting them. It’s not a brilliant reason for eschewing solid food, though is it? ‘You’re fine – you can survive on breastmilk’. I could probably survive on Slim-Fast, but I don’t want to” (page 96).
What a can of worms! First she claims it’s a “fact” that four month olds need more than breastmilk; then she neglects to acknowledge exactly
why paediatricians recommend not introducing solids until 6 months (triggering allergies being a prime motivator); then she likens breast milk to Slim-Fast: a cows-milk-based chemical formula not unlike - wait for it - infant formula (the irony!)
Williams finishes the chapter with one of the most toe-curling, piss-boiling, dismissals of breastfeeding studies I have seen in print. She begins:
“In fact, the case for breastfeeding is not that strong, and it has passed so seamlessly into the book of What’s Best for Baby that it’s often very lazily put” (page 90).
What is this dogma that Williams speaks of?
“The evidence is mild: the statistics showing less asthma, less eczema, less obesity, fewer ear infections: these haven’t been adjusted for social class and environment” (page 92).
Clearly Williams’ is banking on her readership’s ignorance when she writes this drivel. A simple Pubmed search brings up numerous scientific peer-reviewed studies where the results are adjusted for social class and environment (and other confounders)
and STILL declare breastfeeding to be the better choice. Here are just a few:
- Beaudry, 1995, Relation between infant feeding and infections during the first six months of life.
- Nafstad et al, 1996, Breastfeeding, maternal smoking and lower respiratory tract infections.
- Scariati et al, 1997, A longitudinal analysis of infant morbidity and the extent of breastfeeding in the United States.
- Quinn et al, 2001, The effect of breastfeeding on child development at 5 years.
- Williams et al, 2001, Stereoacuity at age 3.5 y in children born full-term is associated with prenatal and postnatal dietary factors.
- Richards et al, 2002, Long-term effects of breast-feeding in a national birth cohort: educational attainment and midlife cognitive function.
- Oddy et al, 2003, Breast feeding and cognitive development in childhood.
- Karlson, 2004, Do breast-feeding and other reproductive factors influence future risk of rheumatoid arthritis?
- Arenz. 2004, Breast-feeding and childhood obesity.
- Martin et al, 2004, Does breast-feeding in infancy lower blood pressure in childhood?
- Victora et al, 2005, Breastfeeding and school achievement in Brazilian adolescents.
- Sørensen et al, 2005, Breastfeeding and risk of schizophrenia.
- Vohr et al, 2006, Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age.
- Taveras, 2006, To what extent is the protective effect of breastfeeding on future overweight explained by decreased maternal feeding restriction?
- Mayer-Davis et al, 2006, Breast-feeding and risk for childhood obesity.
- Scholtens, 2008, Do differences in childhood diet explain the reduced overweight risk in breastfed children?
- Alati et al, 2009, Early weaning and alcohol disorders in offspring.
- Griffiths, 2009, Effects of infant feeding practice on weight gain from birth to 3 years.
- Ogbuanu, 2009, Effect of breastfeeding duration on lung function at age 10 years.
- De Onis et al, 2009, WHO growth standards for infants and young children.
- Tarrant et al, 2010, Breast-feeding and childhood hospitalizations for infections.
- Pisacane et al, 2010, Breastfeeding and risk for fever after immunization.
- Veena et al, 2011, Glucose tolerance and insulin resistance in Indian children: relationship to infant feeding pattern.
- McCrory and Layte, 2011, The effect of breastfeeding on children's educational test scores at nine years of age.
- Evelein et al, 2011, The association between breastfeeding and the cardiovascular system in early childhood.
- Oddy et al, 2011, Breastfeeding and early child development.
- Fisk et al, 2011, Breastfeeding and reported morbidity during infancy.
- Whitehouse et al, 2011, Duration of breast feeding and language ability in middle childhood.
- Van Rossem, 2011, Is the association of breastfeeding with child obesity explained by infant weight change?
- Tozzi et al, 2012, Effect of duration of breastfeeding on neuropsychological development at 10 to 12 years of age in a cohort of healthy children.
- Tharner et al, 2012, Breastfeeding and its relation to maternal sensitivity and infant attachment.
- Jedrychowski, 2012, Effect of exclusive breastfeeding on the development of children's cognitive function.
(You might want to bookmark that list for next time a formula feeder chants the immortal phrase "correlation is not causation!")
Not content with denouncing breastfeeding studies, Williams then turns to subtle racism:
“In its aftermath, breastfeeding makes your tits look like bananas in a Waitrose bag, and dead right, while you’re doing it, it interferes with sex. I have just taken a look at my left breast. If I had one ounce, seriously, 28 grams less restraint, I would take a picture of it and post it on the internet. I don’t want to whine, so I’m not going to describe it in detail; let’s just say that if I found myself in the Amazon, and I wanted to join one of their world-famous ladies’ archery tribes, ain’t nobody be asking me to cut anything off” (page 93).
This is obviously a cryptic attempt at a joke. I’m not such which is more amusing – the fact she expects us to laugh at ethnic tribes or the fact that she uses the sentence, “I don’t want to whine”. If Williams adhered to her own claim, the contents of this book wouldn’t fill a postage stamp.
So after ridiculing tribes women, Williams’ then turns to the WHO (not the rock band):
“My sister said breastfeeding was a tacit World Health Organisation strategy to bring down the global population, since you can’t get pregnant while you’re nursing. Although actually you can, but never mind that. I thought, bollocks: it’s just a pub argument, amplified to the level of policy, where the less evidence you’ve got, the nosier you are” (page 94).
Williams’ is referring to lactational amenorrhoea. In case you don’t know what that means, she provides a ‘helpful’ definition:
“Breastfeeding provides prolonged lactational amenorrhoea. Which means you don’t get your periods back while you’re doing it. That’s it. This is not about existing babies – this is about contraception. My sister was right. We’re being fed this line for the sake of a population curve in places where they have no access to contraceptives!” (page 96).
Oooooh the conspiracy! But wait – before you call the FBI - Williams is missing the point. Lactational amenorrhoea has many benefits, even for rich Western women. These include protection against anaemia and reduction in the risk of developing various cancers including breast and ovarian cancer. These facts are no doubt enough to make Williams choke on her Tampax.
She then goes on to describe a memory, in which her eldest child had an accident resulting in a hospital stay. Williams had a baby at the time, whom she took home and left with her mother:
“And the nurse goes, ‘we do support breastfeeding mothers you, know. You can bring the baby back in – we do support you in your breastfeeding’. I’m not having a rant about the nurse, it just seemed so strange. All your thoughts are on your eldest child, who could have seriously injured himself, and they’re still on about the nutritional superiority of sodding breastmilk! Which they have totally overstated in the first place!” (page 98).
So a medical professional trying to support and accommodate Williams makes Williams throw her toys down in paddy. This is about as coherent as her closing remarks:
“If you breastfeed you’re a bit of a twat - like a fool who believed the headmistress when she said you had to wear a bobble hat, and now you’re making everyone else look bad, and you’re also standing there in a bobble hat” (page 99).
Sisters! You’re letting the side down by breastfeeding! You make the rest of us look like dicks! Show some solidarity!
Each of the books I have looked at here have several things in common: a love of low-touch, high-control parenting, a hatred for breastfeeding, and disdain for babies who dare to encroach on parental well-being. Babies are seen as calculated oppressors and the vaccine against their disease of manipulation is to break their will by installing a regimented routine, preferably from birth.
Why do books like this exist? Answer: They sell! Books that promise an easy plan to an effortless parenthood sell quickly, so greedy bastards keep writing them, and I end up needing dentures from chronic teeth grinding.
Know of a book which needs to be ripped a new asshole?
Email me.



















































































.jpg)


























































































































































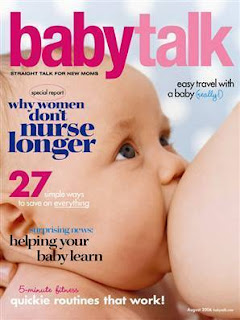










.jpg)


