↧
Breast and Formula Feeding Over Time
↧
Formula Feeding as a 'Choice'
I would like to share with you, a rant I found on Mumsnet today. It was titled, "Women are Stupid":
"Elsewhere, there is a complaint about being unsupported when breastfeeding. This is a feminist issue - and the fault lies fairly and squarely at the feet of women.
I am astounded that after the battles fought in the seventies and eighties, women have allowed such regression.
Look how stupid women are today. They have their bodies surgically adapted to men's fantasies - breasts enlarged, labia trimmed - they bleach their hair, tattoo their eyeliner and lipstick and have themselves spray-painted. They remove their pubic hair so they look like children for their (multiple) partners. If you read about it in a book on social anthropology you'd be horrified at the 'oppression' of women. But women think they are choosing this!
Then they say 'oh, its not fair, no-one supports me when i'm breastfeeding'. Too damn right they don't. Because you and your compatriots have allowed everyone to see you as barbie dolls to use and abuse. They don't want to see you being women, being grown up, feeding your babies, that spoils the fantasy. You created this; live with it.
When you've finished screaming at me about your 'rights' to have your mons pubis decorated with fake jewels and to have your isabella piercing, organise yourselves.
Wash your faces, let the fake tan fade, cut off your dyed hair and let it grow back naturally, so your babies can recognise the human being their genetic memory was expecting to find here. Stay free from chemicals that mask your natural odours, so your babies can recognise you by smell. If people are pressurising you to 'go back to work' say, 'certainly. When this baby chooses to stop breastfeeding'. That gives you four to five years at home, maybe longer, when you are doing something no-one else can - being your babies' mothers."
It may be abrupt and 'out there' but it got me thinking about how infant feeding is a feminist issue, and in particular, it got me thinking about the issue of 'choice'.
I believe a significant part of Patriarchal culture is the brainwashing of women into believing they are making 'free choice'. However in reality, all these supposedly free choices are merely parroted human responses to decades of social conditioning. Take applying makeup for example. The common mantra is that women apply makeup for themselves, yet 90 per cent of British women won't leave the house without applying it (Michaels 2012). What does 'doing it for ourselves' actually mean? One Mumsnetter put it wisely when she suggested, "to me it means we have so inculcated the norms of the male fantasy society that we no longer have our own notion of a desirable self."
Could the same theory be applied to 'choosing' formula? Common reasons women give for rejecting breastfeeding include:
- they don't want their breasts to sag.
- they see breasts as exclusively sexual.
- their husband is uncomfortable with breastfeeding.
- they are uncomfortable with breastfeeding.
- they don't want to breastfeed in public.
- they want to 'get their body back'.
Much of this discomfort springs from the fact that breasts, and in particular breastfeeding, disrupt the border between motherhood and sexuality. Many women cannot cope with the dual-functionality of their breasts. When a woman is desperate to "get her body back," to return to "sexy," to "be her husband’s again" she is consciously or subconsciously trying to appease the notion that her breasts are the property of the male gaze and have to be "good enough" for men again. She is buying into the idea that one cannot be maternal (madonna) and sexual (whore) at the same time.
A choice laced with fear
She has a good point. The choice to formula feed is made in a climate in which women harbour mistrust, disdain, and even fear of their bodies. Like those who dare not leave the house without camouflaging their faces with makeup, when feeding their babies many women believe nature needs a constant helping hand. As women we seldom have confidence in our bare naked selves. Our natural state is to be is feared, seen as faulty and insufficient.
On the topic of rejecting nature, someone called 'Sam' left a fascinating comment on one of my previous articles (here). Her comment is worth reproducing in its entirety:
"Breastfeeding is not a "choice". You can "choose" NOT to breastfeed, but breastfeeding is just the normal thing to do next, once the baby is born. It's like saying you "choose" to placenta-feed. Nope, while the baby is in utero your body just gets on with it and the baby is nourished. There is no "decision" involved. Then the baby comes out and breastfeeding is a continuation of that. You can "choose" to disrupt that continuum. That is your right. Let's just be honest about it and call it what it is."
Her placenta analogy highlights the undeniable fact that birth and breastfeeding are designed to exist on a continuum, and the body of the mother during pregnancy and breastfeeding is the natural 'habitat' of the baby. No amount of technology will improve on this biologically determined pattern. If we see formula feeding for what it really is - a deviation from the norm, rather than a 'choice' - then we can bust the myth that formula feeding is somehow feminist; that brandishing a bottle is liberating.
Rights Vs Choices
In reality, breastfeeding is a maternal and child health imperative and reproductive right. However, rather than being respected as a right, our culture frames breastfeeding as a consumerist and lifestyle choice. The Feminist Breeder has rightly noted that:
"When a biological function is viewed as a 'choice' being made by an individual, society easily decides that it has no vested interest in supporting that 'choice.' If society has no vested interest in supporting that choice, then it’s no wonder a Judge recently ruled that employers can fire breastfeeding mothers. The judge thinks it was the mother's “choice” and the company was not obligated to support it."
Framing breastfeeding as a 'choice' weakens legal protection for breastfeeding families. A lot of women are economically forced into employment in order to feed their families yet are legitimately denied pumping breaks. In this set-up, breastfeeding becomes no more than a privilege disguised as a choice.
How informed is your 'choice'?
One of the most prolific and powerful architects of the pervasive shift from 'right' to 'choice' is - you guessed it - the formula industry. Formula companies use emotional rhetoric to focus on mothers' feelings and intuition rather than knowledge in making decisions. In their marketing propaganda, formula companies cloak and draw attention away from what is actually important in infant feeding. For example, in some of their articulations, love is more significant than breast milk or formula. Their argument is that it is love that counts in infant feeding and care, not what goes into the baby. We see how ludicrous this displacement strategy is when we consider how we would we feel if the tobacco industry used the same argument: "It doesn't matter if you smoke in front of your baby, as long as you love them".
Another, perhaps even more insidious, formula company strategy is to provide 'information' about breast and bottle feeding under the premise of 'helping' mothers to make an informed choice. This 'service' comes in the form of pamphlets, websites, advertorials in magazines, new baby packs, telephone carelines and even assimilated via the bating of health professionals. However when we examine more closely the content of this 'information' we notice how the material is tailored to exploit mothers' fears regarding their breast milk supply, or concerns regarding their partners' ability to bond with their baby (for examples, see my article, "15 Tricks of Formula Companies").
What about Feminism?
Formula companies even leach off feminist notions of liberty, appropriating the discourse of personal choice and female empowerment. A noteworthy example is Elisabeth Badinter who wrote a provocative book called 'The Conflict'. In her book, Badinter argued that if women were to stop breastfeeding and give their babies formula, their economic and social status would rise. However unbeknown to her readers, Badinter holds a controlling stake in and is the board chair of the p.r. and ad agency Publicis, which represents formula makers Nestle, Similac and Enfamil.
The reality is that breastfeeding mothers are less dependant on medical professionals and commercial products, which refutes Badinter's assumption that formula is 'liberation in a can'. Her equation of formula with women's commercial freedom is a grossly false quasi-feminist gesture. It panders to a Patriarchal economic set up in which mothering is devalued and male ways of living are seen as the norm, femaleness as a deviation; A culture where bread-winning is revered, child-rearing belittled, where the functioning of women's bodies is shameful, where pills are dished out to dry up the milk supply of new mothers and where men are more than happy to hand out formula whilst simultaneously lining their pockets. This doesn't sound very feminist to me.
In fact, history has shown us that when women give up breastfeeding, this does not lead to an increase in their employment. In the 1950s, when mothers were encouraged by formula companies and pediatricians to bottle-feed their babies, there was no huge influx of female employees flooding the workforce. Even in contemporary times, "choice" in infant feeding has not created equality in the workplace nor has it liberated women from the burdens of maternity. As I said in a previous article (here), even in contemporary society, it is still mothers who have to take time off from employment to care for their sick formula-fed child.
Despite being fundamentally flawed in these ways, the dialogue of empowerment has been transmitted, like a virus, from formula company to formula feeder. Mothers who chose not to breastfeed assimilated this brand of "choice feminism", soaking it up like a sponge. The rhetoric of 'choice' enables these mothers to rest more easily with their guilt by hiding behind a cloak of 'liberation'. It enables them to argue that even anti-feminist behaviours such as formula feeding are feminist because "feminism is about choice." This approach has slowly caused the phrase "It’s my choice" to become synonymous with "It’s a feminist thing to do" - or, perhaps more precisely, "It is anti-feminist to criticize my decision."
Yes, feminism is about choice but one needs to be honest about the fact that feminism, and indeed parenting, is also about making certain types of choices, whether or not we like to admit it. Individual freedom is to be encouraged - but with one very important caveat - so long as it does not bring harm to others. This is reflected in law. We have the right to free speech, but not hate speech. We have the right to smoke, but not to force others to smoke passively. However during infancy the issue is less defined; a woman’s rights become tied to that of her child. The dialogue of "choice" fails to take in to account those who actually have the most at stake: the child, who may feel the effect of the mother's decision for the rest of their lives.
Feminism is not about reassuring individual women that they haven’t chosen badly. If you choose to hand over your control to medical professionals, to line the pockets of men, to surrender your baby's health to the will of corporations who have no vested interest in your baby's well-being, to contribute to the restriction of women's breasts to the sexual domain, to increase your own, and your baby's risk of cancer and obesity - according to your logic that means that the formula companies, the poorly informed health professionals and the sabotaging family members aren't misogynistic, because anything you as a woman choose to do is feminist. In fact, apparently the real misogynist is the feminist who’s trying to tell you that formula feeding isn't optimum.
A further irony is that, rather than being empowering and 'feminist', the discourse of "choice" operates to stratify mothers into categories of good and bad choosers (i.e. good and bad mothers). The pressures felt by defensive formula feeders – who feel that others look at them as if they have made a "bad choice" – are a legacy of the way choice rhetorically operates in relation to motherhood, functioning to distinguish mothers who choose well from those who do not. Formula company marketing material responds to this perceived stigma by suggesting that women choose well when they use their emotions. All choices, when made from the "heart," are good choices, especially when women make choices perceived to be detrimental from a medical point of view.
Making the Personal Political
Those who champion 'choice' in infant feeding (the "It's my choice and no one's business" brigade) are often motivated by a fear of politics. They hold a worldview that does not challenge the status quo. Instead, any and all choices women make are seen as equally valid, cherished, and beyond judgement. This rhetoric of 'choice' in infant feeding is troublingly tied to and reflective of trends toward hyper-individualism and hyper-consumerism (unsurprising considering its appeal in American and British society); the choice rhetoric tends to neglect the *contexts* (political, institutional, economical) of actual choices; it relieves women of the responsibility of considering the broader implications of their choices (by pretending that individual choices have no social consequences). It’s about making every woman feel good about whatever she does, and treating women like delicate wallflowers who can’t be criticized. In short, the 'choice' rhetoric enables mothers to sidestep the difficulties of making the personal political: i.e. making judgements and demanding change of health professionals, formula corporations, the media, employers, friends and family. Yet, as I explained in my article, "Why the Way You Feed Your Baby is MY Business", infant feeding is inevitably, inherently and unavoidably political.
Politics takes courage - courage to be unpopular, to say what one thinks, to be criticized. We should encourage judgements about the value of different choices, encourage being publicly accountable for our choices, and encourage discussion about which choices should be valued and which are illusions. 'Choice' is an important part of having sovereignty over ones own body and ones parenting, however it is only a part of it and can be completely irrelevant if the context in which choices are being made is not also assessed. Our 'choices' do not happen in a vacuum.
Whatever aspects of being a formula feeder work for you, enjoy them. But don’t fool yourself that you’re doing so of your own unconstrained free will. Your choices are being made in the context of a bottle-feeding culture. You may be doing what you love, but you’re also doing what you’re told. Lactivists who want to fight for your ability to reject patriarchal standards of what is 'decent' breast exposure or who want to ban the ability of formula companies to corrupt health professionals - are trying to give you more genuine, valid, supported options.
Next time you find yourself muttering the hyper-clichéd words, "I support a woman's choice to feed her baby however she likes", stop and think. Your choice rhetoric:
- obscures the fact that formula feeding is a deviation from the norm.
- contributes to the illusion that breast milk and formula are on an even keel.
- weakens legal protection for breastfeeding ('choices' are weaker than 'rights').
- fuels Mother Vs Mother dialogue ('The Mommy Wars').
- relieves formula companies, health professionals and poor support systems of their responsibility (instead all responsibility is placed on the choice-maker).
- discourages individual social responsibility.
- sees women as weak and unable to field criticism.
- shuts down debate, discussion, activism and progress.
↧
↧
Timeline of Breast Changes in Pregnancy
Note: This timeline uses the medical format for calculating pregnancy weeks. So for instance, you technically ovulate near what would be called week two of pregnancy, and your due date is week 40. Notice how breast changes to prepare for breastfeeding occur as early as pre-ovulation!
Week 1:
- During each menstrual cycle, maturation and the rapid growth of milk ducts and alveolar buds take place during the follicular and ovulatory phases.
Week 2:
- These changes to your breasts (maturation and the rapid growth of milk ducts and alveolar buds) peak in the late luteal phase of your menstrual cycle. It is at this time that your egg is fertilised and embeds itself in your uterus.
Week 3:
- For some women, tender breasts begin as early as a few days after conception. The sensations are often most noticeable down the sides of the breasts. This is because the internal mammary artery runs down the medial side of each breast and this supplies the majority of blood to the breasts.
Week 4:
- Tingling and pricking, particularly around the nipples, due to an increased blood supply. Avoid wearing a bra with seams across the nipples or lacy cups, which can also irritate the skin.
- Your breasts may also tingle with temperature change.
Week 6:
- Nipples become more prominent.
- The areolae – the areas of skin around the nipples – start to darken in hue due to an increase in natural pigmentation. This colour change is believed to be nature's way of making the nipples visually easier for the baby to find for feeding.
- Your breasts may become fuller and slightly uncomfortable, perhaps similar to the way they feel pre-menstrually. This is due to the combined and continued action of the hormones (oestrogen, progesterone, and human placental lactogen) that are responsible for the growth of glandular tissue.
- Your milk ducts are already beginning to swell in preparation for lactation.
Week 7:
- An increase in breast growth and weight is usually the most obvious physical sign of pregnancy at this stage. Some women gain well over 680g (1.5 lbs) in each breast (Fredregill 2004). It is caused by the production of oestrogen and progesterone from the corpus luteum (what is left of the follicle after ovulation) and the growing placenta. These pregnancy hormones encourage fat to be laid down and milk ducts to grow. Breast tissue extends up into the armpit and some women with additional breast tissue (accessory breast tissue) may find that this also gets bigger in size.
- The alveoli expand and begin forming distinct lobules (see diagram).
Week 8:
- Your breasts may feel tender, sore and nodular due to hypertrophy of the alveoli (increase in volume).
- Blood vessels may be quite visible just under the skin of the breasts. This network of delicate bluish veins is developing to house your increased blood supply. Their appearance is often vivid on fair-skinned women and sometimes not even noticeable on darker women or women who are overweight.
- Small bumps which look like little pimples around the nipples, called Montgomery’s tubercles begin to appear. These hypertrophic sebaceous glands will secrete an oil that keeps the skin supple and discourages bacteria, and there may be between 4 and 28 around each nipple. In fact, this is one of the most reliable signs of a first pregnancy, but since they do not shrink completely after pregnancy this cannot be depended on as a diagnostic sign for subsequent pregnancies.
Week 9:
- The areola undergoes further darkening and may enlarge in diameter and become more erectile. Women with darker hair and complexions generally experience more noticeable changes than fair - skinned, blonde or red - headed women.
- An outer ring of lighter-coloured tissue called the secondary areola starts to appear (see photograph).
- It is very important that you perform regular breast examinations now. Fortunately, breast cancer is uncommon in women under 40, but when it does develop in younger women, the tumour is usually oestrogen dependant, which means that pregnancy can greatly accelerate both the local growth and distant spread of the abnormal cells (Regan 2005).
Week 10:
- Breast tenderness is likely to continue this week.
- Montgomery’s tubercles increase in prominence.
- You have just passed the first period of major breast growth. Therefore now is a good time to get professionally measured for a larger bra. Make sure that it has good support all the way round, including the underarm and back sections, and that it is not underwired.
Week 12:
- If you have had cosmetic breast implants you may be feeling especially tender now. This is due to your own breast tissue is growing around the implant. The skin over the breasts may feel taunt and uncomfortable too.
Week 14:
- Your breasts will be fuller and heavier as a result of increased circulation.
- The areola may become even more deeply pigmented and slightly speckled. Some patches may seem darker than others. This darkening will fade but not disappear entirely after birth (Murkoff 2009).
Week 16:
- Continued enlargement of areolas.
- Glandular tissue undergos further change - the alveoli sacs now start to become lined with special milk-producing cells (called 'acinar' cells).
- Colostrum may be expressed. This is a sweet, sticky, highly-nutritious fluid that will feed your baby until your milk comes in a few days after delivery. Colostrum contains sugar, protein and antibodies – in fact, all your newborn’s nutritional needs. At this stage the colostrum is usually thick and yellow.
- A few women may begin to get occasional leakage of blood from the nipple. This is due to the increased number and sudden growth of blood vessels.
- Drops of blood may also be seen on the bra because the sticky colostrum temporarily 'glues' the nipple to the inside of the bra and a tiny bit of nipple skin is removed with the bra, which does heal. Although this can be normal during pregnancy, it is best to get any leakage of blood from the nipple checked by your midwife.
- The secondary areola develops with further extension of the pigmented area that if often motted in appearance.
- Breast tenderness may have diminished now.
Week 18:
- You are accumulating fat stores in your breasts but the majority of the extra weight is currently made up of the increase in blood volume.
- Some women may find a lump appear around this time. The most common ones are cysts (fluid-filled sacs), galactoceles (milk-filled cysts) and fibroadenomas (fibrous tissue). If you already have a fibroadenoma you may find this gets bigger during pregnancy. The vast majority of breast lumps in pregnancy will be benign (not cancer). However, it is a good idea to get any new breast lump or growth of an existing lump checked out by your doctor and to tell your midwife if you have an existing fibroadenoma, cyst or any other breast problem (NHS UK 2012).
Week 20:
- By now, you may have a scattering of stretch marks, particularly on the underside of your breasts. The vast majority of women will develop stretch marks on their breasts during pregnancy (Regan 2005). These are caused by the collagen beneath the skin tearing as it stretches to accommodate your enlarging breasts. The number and extent of stretch marks varies greatly from woman to woman and is determined mainly by your genes and your age (as you get older your skin loses its elasticity, making stretch marks more likely).
Week 22:
- The second period of major breast growth has occurred and you have probably noticed a dramatic change in the size of your breasts. If so, it’s a good idea to be professionally measured for a new bra (yes, another one). Stay clear of underwiring as this may restrict blood supply and crush the developing milk ducts. Choose a natural fabric such as cotton rather than synthetic, as you are likely to sweat more than usual.
Week 26:
- Your breasts are becoming fuller and, in some women, they may become more pendulous.
- You may notice from this stage onwards that you leak colostrum at random times, like during sex or when you are in the bath. Having said that, don’t worry if you do not see any colostrum throughout your entire pregnancy. It is there, it is just that you are one of the fortunate women from whom it has not actually leaked out.
Week 27:
- By now your breasts are sufficiently developed to be able to function as milkproducing glands (called lactogenesis) (Neville 2001), however, the elevated plasma levels of progesterone prevent the breasts from secreting mature milk until days after the placenta is delivered.
Week 28:
- You will probably be able to see the blood vessels that lie just below the surface of your skin quite clearly now, as the volume of blood circulating around your body increases further.
- Continued darkening of the nipples, as the amount of skin pigmentation increases.
- Milk ducts begin to dilate.
- You may already have bought a bigger bra by now. Don’t buy more than one of two with each size change, as they will only fit for a limited time.
Week 30:
- Nipples may become more prominent due to increased progesterone production.
- You may find that you suffer from what is known as ‘sweat rash’. This occurs because a higher than normal proportion of your blood flow is going to your skin and mucous membranes and their blood vessels have become dilated to accommodate it. Check that your bra is not too tight. Go for a re-fit if necessary, and choose a cotton bra. Talcum powder can help. Also try to get some air to the area whenever possible. If the problem persists, see your midwife; the rash may be due to a thrush infection and an anti-fungal cream may be needed.
Week 32:
- The areolas will have broadened and darkened considerably now.
- You may find that small amounts of creamy fluid ooze from the Montgomery’s tubercles. Avoid using soap on your breasts, as it may remove this valuable sebum and leave the skin dry.
- By now the skin around your breasts may be dry and itchy as it becomes increasingly taut. To reduce itchiness make sure your bras are 100% cotton as this fabric helps to keep the skin cool and enable it to breathe.
- Any stretch marks may become more pronounced.
Week 34:
- As well as leaking a creamy secretion which moisturises your nipples in readiness for breastfeeding, you may also leak a little colostrum from around now. It is sometimes accompanied by a tingling, fizzing sensation.
- Progesterone now causes the nipple to become more prominent and mobile.
Week 36:
- The NHS suggest that this is the best time to be fitted for a nursing bra (rather than generic pregnancy bra) as your breasts will have done the majority of their growing by now. The bra fitter should take into account that your breasts will get even bigger when you start producing milk, but will probably settle down again later. The fitter will probably suggest going up one or two cup sizes to allow for this (NHS UK 2012).
Week 38:
- As delivery approaches, your colostrum will turn from thick and yellow to pale and nearly colorless.
Week 40:
- Getting impatient? Hand manipulation of your nipples causes your body to release the hormone oxytocin which can stimulate contractions. This could not occur in early pregnancy because the hormonal changes which cause the uterus to be sensitive to oxytocin only begin late in pregnancy.
Delivery:
- Congratulations! Labour and delivery start a physiological chain reaction. After delivery of the placenta and membranes in the third stage of labour the levels of circulating oestrogen and, specifically, progesterone fall and levels of prolactin increase. At the same time, nerve impulses from the uterus travel to your brain's hypothalamus gland. The brain then signals the pituitary gland to release the hormones prolactin and oxytocin. This stimulates your breasts to start lactating, initially producing colostrum for the first couple of days post birth and then, as its composition alters, increasingly mature milk.
- Your nipples 'toughen up' after 2 to 3 weeks of breastfeeding (Cave and Fertleman 2012).
Important note:
A minority of women notice no significant change in their breasts until their milk comes in, around three days after delivery of their baby. Some find that the expansion takes place so gradually that it’s not perceptible. As with all things in pregnancy, what’s normal is what’s normal for your breasts. You may be concerned about insufficient glandular tissue (IGT) or breast hypoplasia. Don’t worry, though slower growth means you won’t have to replace bras so often, it is unlikely to have any impact on your ability to breastfeed. Studies have found that there is no association between breast growth during pregnancy and subsequent milk production (Hytten 1995, Cox et al 1999). To ease your mind, talk to your midwife or doctor and insist on a breast exam.
↧
Anti-Breastfeeding Books: Part Two
Welcome to what is regrettably another instalment to the literary anti-breastfeeding saga (get acquainted with the first part by clicking here). The books I am about expose are aimed at first time parents and are available mainstream. Their heavily-biased content exploits noob naivety, perpetuates myths, and forces misinformation upon unsuspecting readers. Best get yourself a stiff drink.
Your Baby Month By Month
Su Laurent
Pediatricians and sound breastfeeding advice. Trying to find a correlation between these two things normally gives me a headache. So I needed a lobotomy after reading this.
Aside from examples of glaring misinformation which I will come to later, there are many instances where the author, Laurent, a pediatrician, uses subtle semantics to obscure the risks of formula. Take for example, this caption from page 87:
 |
| (Image and caption from page 87) |
Laurent fails to mention that the reason formula takes longer to digest is because it is harder to digest and an intestinal irritant. This is why formula fed baby’s faeces have a more repugnant smell, and why formula fed babies regurgitate more.
The selectiveness and insidiousness of Laurent’s ‘information’ is even more blatant when you consider the context in which it is given - the sleep chapter. Inside, it claims the sooner a baby gets into a sleep routine, the sooner their parents will get a good night’s sleep. The message = It is easier to put a formula fed baby into a routine, and then you will get more sleep. This has boobie trap written all over it.
Speaking of boobie traps, Laurent has a predictably anti-cosleeping stance, not uncommon for paediatricians:
“Sharing a bed with your baby is not recommended in the early months” (page 65).
However as I explained previously in “Reasons to Cosleep”, sleeping with your baby is actually safer both from a suffocation perspective and from a fire safety perspective. In fact, countries where cosleeping is the norm have the lowest SIDS rate (Palmer 2009). Not to mention of course, cosleeping facilitates effective breastfeeding both practically and physiologically.
After increasing the risk of supply problems by advising that mothers sleep apart from their babies, Laurent exacerbates these problems by advising formula feeds. Page 90 reads:
 |
| Snarky much? (From page 58). |
No mention is made of the fact that giving formula to a breastfed baby will diminish breastmilk supply. Equally, no suggestion is made of the possibility of using expressed breast milk, which would help to preserve supply.
Then we get to arguably the most disappointing chapter of the book, which wholly concentrates on feeding. In this chapter, Laurent commits the cardinal sin of childcare writers – she sneaks personal anecdote into what is claimed to be a factual textbook. On page 186, she declares:
 |
| 'Hands on'. A mother with newborn performing to an audience. (Image from page 30). |
Such subjective opinion has no place in an ‘advice’ and ‘guidance’ manual, other than to perhaps illuminate exactly why Laurent knows so little about breastfeeding. Whilst I’m not going to discuss whether or not professionals should have successful breastfeeding experience in order to act in an advisory role to mothers (you may have your own thoughts on the matter, and you can read mine here), I think it would have been a good idea for Laurent to co-author this book with someone who actually has breastfeeding experience and expertise. Having no experience of surpassing the 6 month mark herself, Laurent has little time for extended-breastfeeding. This is particularly clear from the following quote, also taken from page 186:
“My personal view is that breastfeeding beyond the age of two years is a little odd – this can lead to the spectacle of a child lifting up her mum’s top to help herself to the breast whenever she wants”.
Firstly, why is this a spectacle? Secondly, if the mother was uncomfortable she could easily explain to the child that nursing is for private. As for finding the nursing of a two year old “odd”, I wonder at what age Laurent believes breastfeeding goes from acceptable to “odd”. I fear it is probably 6 months, what she deems to be “the right length of time to breastfeed”, which would of course necessitate the use of formula for another 6 months. Which formula company is lining Laurent's pockets we may ponder.
On the same page Laurent advises a mother whose partner wants her to stop breastfeeding her baby at 12 months:
“Your partner may have been looking forward to having you all to himself again and if that’s the case it’s important to get these feelings out into the open. As far as your baby is concerned, while she gets pleasure from breastfeeding she won’t lose out nutritionally if you decide to wean her”.
In other words, she's advocating forced-weaning. If my partner had such an attitude, I'd advocate a bitch-slap to the head. Sadly the forced-weaning tactic is common in childcare manuals, and this next book is no exception...
The Baby Care Book
Jeremy Friedman and Norman Saunders
This American baby-care manual is another regurgitation from paediatrician authors (this time, a double act). Initially it appears to adopt a politically correct one-the-fence approach to infant feeding. Page 20 introduces the subject:
“Although many people have strong opinions about this choice, both methods are acceptable. Choosing one over the other will not change your relationship with your baby”.
However as you progress through the book, the authors’ bias towards bottle-feeding is unmistakable. Page 292 chirps:
“Most babies love their bottles – and so they should, given how much good nutrition the contents provide”.
The authors are not referring to expressed breast milk here. In fact, it soon becomes apparent that they have an arsenal of boobie traps and scaremongering to give the reader a not so subtle push in the direction of formula.
Take page 69 for example; the authors maintain that:
“healthy full-term babies do not need to be fed immediately”.
This advise is inaccurate and tantamount to sabotage. Babies nurse better straight after delivery, and it is the first few days that lays the hormonal groundwork for a mother’s future supply of mature milk (see ‘Timeline of a Breastfed Baby’). Discouraging initial feedings can have ruinous consequences for a mother’s milk supply. As can discouraging night feedings, which timely occurs on page 106:
 |
| (Image from page 20) |
Okay, bonus points for mentioning pumped breast milk. However there are several red flags in this paragraph. Firstly, we see the age-old myth that fathers need to bottle-feed in order to bond with their babies. Lord knows how fathers managed to bond before the invention of the bottle. How is holding a plastic teat in a baby’s mouth any more bonding than cuddling, bathing, nappy changing, massage, baby-wearing and pretty much any parenting activity? Secondly, placing formula before breast milk in the sentence is a subtle undermining of breast milk. The former is arguably more convenient for the parent, the latter is more favourable for the baby, but this distinction is obscured. Thirdly, and perhaps more importantly, the consequences of bottle-feeding, particularly at night, are omitted. Introducing regular bottles risks nipple confusion. It also risks reducing the mother’s supply, even if the bottle contains expressed breast milk. This is because direct stimulation of the breast through the night regulates milk supply, as the responsible hormones are more acute at night. The book’s absence of this vital information robs parents of the opportunity to make an informed choice, whilst sabotaging their breastfeeding relationship.
Perhaps one of the most worrying examples of sabotage in the book occurs in the section titled, “Failure to Thrive”. The information reads:
 |
| (Image from page 148). |
The fact that the authors who wrote this are professionally qualified paediatricians is concerning. One must wonder how many struggling mothers they have given this advice to. Firstly, a breast pump cannot – ever – give an accurate indication of a mother’s milk supply. The competence of a baby at the breast is far higher than the competence of a breastpump, even a hospital grade electric one (see, 'Top 10 Breastfeeding Boobie Traps'). A lot of women cannot pump much breast milk yet go on to adequately nourish their babies. Secondly, weighing a baby before and after a feed (so-called ‘test weighing’) is inaccurate and has not been recommended since 1994! (Source: La Leche League).
The sabotage continues, perhaps unsurprisingly, in the chapter on sleep, which assures us that, 6 month old babies do not need to feed at night, in fact:
 |
| (Image from page 132). |
So it seems we must manipulate our babies and not “allow” them to feel anything we may deem inappropriate to our lifestyle. This parent-centric approach is echoed throughout the book. For instance, page 112 maintains that:
“Parents will sometimes decide that bottle-feeding their baby is the best option for them. And in many cases, it is”.
One thing is factual about this sentence – bottle feeding is often better for ‘parents’. However it is seldom better for ‘baby’. As this is called “The Baby Care Book” one would assume babies’ needs should be the focus. Obviously not, if page 122 is anything to go by:
“Both breast-feeding and formula-feeding are safe and nutritious ways to feed your baby...”
“Whilst breast milk is the best milk for newborn babies, infant formula is the next best thing. Formula is nutritionally sound.”
“Infants will grow and develop appropriately and will be generally healthy when fed formula”.
Whilst the safety and nutritional status of formula is debatable (see here if you want to go there), one fact that is beyond debate is that formula is certainly not‘the next best thing’. In fact, it comes fourth, after breastfeeding, expressed breast milk, and then expressed donor milk (Newman 2006). Formula is literally a last resort in terms of infant health.
 |
| (Image from page 153). |
“Breastfeeding requires a mother to be with her baby most of the time, which can be limiting, and at times, isolating” (page 125).
“Find ways to breastfeed discretely. There are ‘privacy’ drapes you can purchase that help you cover up when feeding” (page 125).
“Reduced sex drive may be a deterrent for some mothers” (page 126).
Added to this catalogue of breastfeeding disadvantages, the book features a similarly extensive list of “contraindications to breastfeeding”. The text insists that breastfeeding should be discouraged when “the mother has active tuberculosis”. Page 127 maintains:
“For 2 weeks after treatment begins, the infant should be separated from her mother because of the risk of infection”.
This is outdated advice. In the past, infants born to mothers with tuberculosis were sometimes separated, however the World Health Organisation has held that these measures are “no longer recommended” and this has been the case for over two decades! (WHO 1998).
The book claims another contraindication to breastfeeding is when “the mother is HIV-positive” however this age-old myth has been rebutted many times (see here).
A further apparent barrier to breastfeeding is when “the baby has galactosemia”. There is where the infant lacks a critical liver enzyme (responsible for converting galactose to glucose). The galactosemic baby will fail to thrive on breast milk or formula based on cow's milk, so yes, it is true that babies with a severe case of galactosemia should not breastfeed. However - and this is important - galactosemia is an extremely rare condition. It occurs once in every 85,000 births (Riordan 2008), so why did this book feel the need to devote an entire paragraph to it? Whilst at the same time, neglecting to list the dangers of formula? (Baring in mind that formula use is very common). I’m sensing a conflict of interest.
 |
| Contrast this bottle-feeding image (from page 164) with the breastfeeding ones above. What do you notice about the mothers' facial expressions and appearance. |
“Partnership: formula-feeding promotes partnership in caring for the baby. Father’s, grandparents, other family members, and close friends can feed your baby formula from a bottle” (page 128).
“Freedom: formula-feeding offers more freedom for the mother, giving her the opportunity to be away from her baby for an extended period of time” (page 128).
Both of these supposed ‘advantages’ can apply to breastfeeding too, yet they are omitted from the list of breastfeeding advantages. According to this book, breastfeeding has only three advantages for the mother: uterine contractions, weight loss, and lactational amernorrhea. It's worth noting that two of these are temporary. There is no mention that breastfeeding reduces the risk of cancer, diabetes, osteoporosis and cardiovascular disease, as well as the significant advantages to your wallet (see, 'Ten Selfish Things I Love About Breastfeeding').
To add further insult, the section titled ‘bonding’ states:
 |
| (Image from page 173). |
There is nothing about breastfeeding which prevents men from having eye contact and interaction with their babies. This bizarre assumption undermines the intelligence of the book’s readers. It also obscures the fact that there is more bonding involved in breastfeeding than simply enforced eye contact and interaction. A more significant factor in bonding via breastfeeding is the hormonal response in both mother and baby during a feed. This response cannot be duplicated in formula feeding.
If the biased lists of advantages and disadvantages, and the huge list of ‘breastfeeding contraindictions’ wasn’t enough to put off new mums, the instructional section titled, ‘Getting Started With Breastfeeding’ just might have them running to the nearest formula store. The section begins with:
“If you have spoken with any first-time mothers, they may have told you that breastfeeding is anything but natural at first” (page 130).
I see where the authors are coming from. Initially, breastfeeding is hard, however the book used the phrase, “anything but natural” which is quite different from hard. It implies hopelessness and feeds the culture of failure-acceptance I’ve spoken about before (here).
 |
| Kudos to the book for featuring this image of hand expression (from page 147). Shame that it's showing an incorrect technique that will cause friction burns (ouch!) |
The next page is loaded with intricate instructions regarding feeding positions, latch, and paraphernalia. This barrage of information overcomplicates breastfeeding, providing unnecessary hurdles which are likely to intimidate and confuse a new mum. The list of breastfeeding apparatus is particularly excessive, and we are warned to “make sure you have the special equipment”. So what is all this equipment we need to enable us to breastfeed? Page 132 informs us that:
“If you are sitting up to feed, you will likely need a pillow. A special breastfeeding pillow can range in price from $30 to $100. These pillows may require you to use a chair with low or no armrests”.
Then we are told we need a nursing stool:
“Once you are sitting in your chair, with your baby on the pillow, you may need to bend toward your child or even slouch, and one shoulder may lean forward more than the other, all of which can make you very uncomfortable over time” (page 132)
This is false. You shouldn’t slouch towards your child. You bring your baby to the breast, not your breast to the baby. So the authors have created a non-existent problem, and then continue to present a solution. Unsurprisingly the solution involves more financial expense:
“The solution is a nursing stool. Most women, unless they are tall or are sitting in a short chair, require a footrest. You can purchase a specialized nursing stool” (page 132).
So once you’ve purchased the entire stock of Mammas and Pappas, you may want to get down to the business of actually feeding your baby. The book advises scheduling your newborn’s feeds because “infants prefer a routine” (page 151). The authors even go as far as to suggest that, “It can be helpful to use the recommendations for formula-fed babies as a guide” (page 145). “Feed your baby on a time-based schedule. For example, you might choose to feed her every 3 hours from the start of one feed to the start of the next feed” (page 142). This is great advice... if you want to diminish your milk supply and enjoy the sound of crying babies.
 |
| (Table from page 143). |
“Regardless of the approach you adopt, be flexible. Breastfeeding is meant to be easy. If you are feeding your child every hour because she demands it, it will be difficult for you to go anywhere or do anything” (page 142).
Upon reading that I spat out my drink all over my baby, who was chilling in his sling. (You know, slings, the simple pieces of fabric that enable you to go anywhere and do anything – whilst breastfeeding). It seems the authors must be unfamiliar with slings. Could it be that they’re also unfamiliar with diapers? Let me explain with this quote from page 144:
“Unlike formula-feeding, where you know exactly how much formula your baby is taking in, breastfeeding is much less measurable. In fact, it is virtually impossible to know exactly how much your baby is taking in during a feed”.
It’s easy to reassure yourself that your breastfed baby is consuming enough – the answer lies in their diapers. If he is having at least one or two wet diapers each day, his intake is sufficient (see ‘Timeline of a Breastfed Baby’).
So far we’ve been forewarned about a catalogue of breastfeeding miseries, from deflated sex drive to poor paternal bonding, anxiety, isolation, rare birth defects, and $100 nursing pillows. However the authors have one more area of breastfeeding life that they wish to undermine and inject with angst – pumping.
“For some women, expressing breast milk is very simple. They try it a few times and – voila – they are able to produce an adequate amount of milk on a regular basis. Other women have more difficulty. Some complain that they are not able to express very much milk; some find pumping very painful” (page 150).
Woah pumping doesn’t sound too great. Hats off to the exclusively pumping mums. It’s a relief that I can choose not to do it... or can I?
“Babies have a tendency to prefer the feeding method they use most often. To prevent this, introduce a regular bottle once breastfeeding is established. If you don’t routinely offer them a bottle, they might not take it when you want them to” (page 150).
So not only can pumping be ‘painful’ (note: it shouldn’t be), but every mother needs to do it to prevent a fate worse than death – bottle rejection. Mothers are urged to, “offer your child a bottle of breast milk every few days” (page 151). As “babies have a tendency to prefer the feeding method they use most often” there should be no fear about nipple confusion right? (Wrong). However discussion of nipple confusion is absent from the book.
The breastfeeding section of the book comes to a conclusion with a section titled, “Weaning your child”. The book doesn’t use the word ‘weaning’ in the UK ‘introduction of solids’ sense; rather weaning, in this context, means stopping breastfeeding. The section begins:
“Children often wean themselves off the breast between 2 and 4 years of age. However, based on your lifestyle, you may wish to wean your baby before then” (page 152).
 |
| Another dodgy breast illustration (from page 137). Careful love, you'll pull it off. |
But enough sadness. The book now turns from the depressing tone of the breastfeeding section, to a more upbeat formula-feeding section. In the first part, titled, “Getting started with formula-feeding”, the book chirps:
“Relax! It doesn’t take long to become an expert at formula-feeding your infant. Take all the time you need to get things right, then sit back and enjoy feeding your baby” (page 161).
Then under bold font which reads, “Iron and fatty acid fortification”, the book maintains that:
“Recently, formula companies have begun to fortify their formulas with the fatty acids DHA (docosahexaenoic acid) and ARA (arachidonic), which are building blocks for the brain. These fatty acids are found in the systems of breastfed babies but not in those of formula-fed babies” (page 165).
This is true. However what the book conveniently omits to mention is that there is no proven benefit from adding DHA, and possible risks to the DHA claim. The synthesised DHA added to formulas is in a different biological environment to breastmilk, which is a species-specific, living substance. Conversely, formula contains no co-enzymes or co-factors to enable the fats to work optimally. The World Health Organisation has maintained that:
“WHO does not have a recommendation about the addition of docosahexaenoic acid (DHA) to formula milk.....to date no solid evidence exists to be able to say that adding DHA to infant formula will have important clinical benefits” (Baby Milk Action).
After championing the advantages of each type of formula, the book then explores preparation of formula feeds, beginning with the advice, “The correct way to prepare your baby’s bottle is to closely follow the directions provided by the formula company” (page 170).
As incorrectly prepared formula is a major cause of malnutrition and illness, surely the formula companies are duty-bound to supply accurate preparation instructions? It would appear not. Click here to view the NHS instructions for preparing formula. No formula company has given this information to parents, and some directly contradict it (see “15 Tricks of Formula Companies”).
Speaking of incorrect advice, the book’s guidance on introducing solids is potentially harmful: “Generally, it’s best to offer cereal at the beginning of the meal and then ‘top it up’ with breast milk or formula” (page 296). This is the polar opposite to what is best for babies. Breastmilk or formula remains the most important form of nourishment in a baby’s first year (NHS 2007; Better Health Channel 2012; Think Baby 2012). Milk feeds should always be offered first as solid food can displace the amount of milk in a baby's diet.
This book provides incorrect information and biased propaganda to breastfeeding and formula-feeding mums alike. I find it hard to think of anyone it would be suitable for, besides the recycling plant. I can think of another book that would also be good for pulp...
Baby’s First Year
Hollie Smith
This book is a bit of a chameleon. One moment it’s praising breastfeeding, the next moment it’s contradicting it. The book is set out as a timeline, with each chapter focusing on a month of baby development. Chapter one (newborns) begins with what can hardly be described as a glowing appraisal:
“At the outset, breastfeeding can be really hard work, it’s true. Your nipples can get extremely sore and, in the early weeks, the sheer amount of time babies want to suckle can be draining. On top of that are the emotional factors – the worry that she’s getting enough milk, and the guilt if you don’t think she is” (page 15).
Then we are told that breastfeeding mothers should watch their consumption of “spicy dishes, vegetables such as cabbage, broccoli, onions and sprouts, and acidic fruits or juice” as these can apparently make baby “excessively windy, uncomfortable or colicky” (page 20). The facts however (which let’s face it, is all a childcare manual should be interested in) are that a mothers diet is rarely problematic to her breastfeeding relationship (San Diego Breastfeeding Collation 2002; Kellymom 2011; Baby Center 2012). Think about it – women in South America who eat lots of peppers, or women in India who eat lots of curry don’t have babies any more colicky or fussy than babies in the UK or US. As for “gassy” foods like cabbage, broccoli and sprouts making a baby windy, that’s one of many breastfeeding myths. Gas is produced when bacteria in the intestine interact with the intestinal fiber. Neither gas or fiber can pass into the bloodstream, or into your breastmilk, even when your stomach is gassy.
Another breastfeeding myth can be seen on the same page: “It’s not a good idea to smoke if you’re breastfeeding, because traces of chemicals, including nicotine, can pass through to your baby” (page 20). The reality however, is that a mother who can't stop smoking should still breastfeed. Breastfeeding provides many immunities that help a baby fight illness and can even help counteract some of the harmful effects of cigarette smoke. The pros outweigh the cons (Dorea 2007; Batstra 2003; Nafstad 1996).
After this disappointing start to the book, things go from bad to worse in the next section which quotes mothers' experiences:
“I was determined to breastfeed. However I found it incredibly difficult and painful, and then developed mastitis in both sides. At that point I decided to give both me and my son a break and move to formula” (page 23).
“I went back to work part-time when my second was seven months so I expressed for a while, but that was very hard work so I switched to formula. Challenges to feeding after six months include the fact that my babies often woke in the night and nothing would get them back off again. Also, feeding in public can be harder... Also teeth can be an issue – I was once bitten so hard in public that I screamed and was left bleeding” (page 198).
“I stopped at around 13 months because from that point they could have cow’s milk, their sleep patterns had matured and I wanted to be able to go out or have a night away sometimes. I also felt that, in order to convince others that breastfeeding is a normal and OK thing to do, I didn’t want to be seen as extreme or lactivist” (page 198).
“I loved breastfeeding, but my daughter was a very hungry baby. By six months she was having a feed in the morning only, and one day she just didn’t seem to want it and so I stopped altogether, bought a bottle of wine, had a hair cut and went out and bought new bras. I was ready to stop, and for me it was symbolic. I was getting my body back” (page 198).
“I didn’t want to be feeding still when they were walking – just something I was not comfy with. I also wanted my body back – and some sleep!” (page 199).
 |
| (Page 23). |
Don’t get me wrong, I’m all for lifting the veil on breastfeeding - the veil of romanticised maternity which depicts breastfeeding as an all-easy, all-blissful lovefest. Women need to know the reality - the inconvenience, the relentlessness, the initial discomfort. However such information is only useful when it is accompanied by guidance on how to overcome these breastfeeding hardships, and indeed, a statement that they can be overcome. The impression given in this book is that if breastfeeding is painful, if you get mastitis, if you go to work, if your baby reduces feeds, or if your baby has had a birthday - it's time to stop breastfeeding. This disappointing message is no surprise given how uninformed the author, Smith, appears to be. In the “6 months” chapter, she states:
“If you’re still going strong with breastfeeding now, that’s fantastic! You’ve made it to the end of the recommended period and you can feel certain that you’ve given your baby the best possible start in life” (page 197).
Breast is not the best start – breast is the normal start in life; but with that discrepancy aside, it concerns me that Smith advocates 6 months as the end of when breastfeeding is recommended. No mention is made of ‘6 months exclusive breastfeeding then solids introduced with continued breastfeeding’ which is what the World Health Organisation, Unicef and the Department of Health of every country on the planet recommends. Likewise, no mention is made that WHO guidelines recommend breastfeeding till at least 2 years. Instead, Smith gives the impression that it is normal for babies to move from breast to formula at this point. Her lack of knowledge is further evident on the same page when she declares that:
“It’s normal for breastfed babies to self-wean (drop the feeds naturally) when they’re ready, at some point between six months and two years” (page 197).
Inaccurate information regarding self-weaning seems to be commonplace in anti-breastfeeding books; as I mentioned above in my critique of The Baby Care Book, the worldwide average age of weaning is 4.2 years (Dettwyler 1996) - a far cry from 6 months. Furthermore, true self-weaning before a baby is a year old is very uncommon. In fact, it is unusual for a baby to wean before 18-24 months unless the mother is encouraging weaning (Bonyata 2011). Thus it seems bizarre when, on page 199, Smith quoted a mother saying:
“The last feed to go at ten months was the evening feed – when Alice ditched me of her own choice, I’m afraid!”
Clearly this mother was misreading her baby’s signals, yet Smith quotes this as a common example of self-weaning. The baby in question was still too young to drink cow’s milk, and yet milk is the main staple of a baby’s diet until 12 months. So that necessitates a move to formula. Infants consuming a man-made chemical concoction is obviously not what nature intended, hence the child did not self-wean.
More misreading of nature can be found later, on page 243, under the title “Saggy Boobs”. Yes, like a fart in an elevator, this myth refuses to die:
“Sagging boobs (the medical term is breast ptosis) are an unfortunate but very normal consequence of motherhood. As the breasts swell during pregnancy and breastfeeding, the ligaments and tissues that support them are stretched”.
Equating sagging breasts to breastfeeding is the oldest, most common, most tiresome breastfeeding boobie trap. Pregnancy causes breasts to sag, Smith got that correct. However including by breastfeeding in the mix, Smith suggests that a woman can reduce the severity of sag by not breastfeeding – which is 100% not true.
Another classic breastfeeding boobie trap concerns the introduction of solids. Like The Baby Care Book reviewed above, this book also recommends prioritising solids over breastfeeds:
“Too many breastfeeds can affect appetite, so avoid offering the boob before mealtimes... You’ll need to make sure she gets other dairy products, such as cheese and yoghurt, as it’s impossible to know if she’s getting sufficient quantities of breast milk to get the same level of nutrients that these foods provide. And it’s still important that she learns to drink from a cup, so be sure to offer her water in her beaker with meals and snacks” (page 285).
Here we see Smith missing a vital point – breast milk is biologically designed for human babies, whereas cheese and yoghurt, while still nutritious, are man-made foods created using milk intended for baby cows. As breast milk is species-specific it is more bio-available (easily absorbed by the human body) than cheese and yogurt. So if a baby were to prefer breast milk to cheese and yogurt, this is not a travesty. Bear in mind also, that breast milk automatically adjusts to a child's needs as they get older. To displace breast milk (rich in fats and brain-building omega 3s) with water in a beaker (nutritionally void) is not wise guidance.
In conclusion, I can sum up this book in one word – schizophrenic. On the one hand, it tries to be a childcare manual offering “key practical knowledge from the experts”, whilst also presenting itself as a cosy informal chat with “friendly words of wisdom from the members of netmums”. This awkward marriage of medical subject matter and personal anecdote does not lend itself to accuracy and integrity. Speaking of lacking these things, may I present to you, Exhibit C:
Home Made Kids
Nicola Baird
This is a parenting manual with an eco-friendly slant. The introduction begins, “Having a baby can be the perfect opportunity to make practical changes that are good for you and that avoid damaging the planet” (page 1). Excellent, I thought. This will surely lend itself to a pro-breastfeeding stance.
Who was I kidding? Despite its heavy focus on natural child-rearing and caring for the environment, ironically this book does little to encourage breastfeeding. Rather, it paints a picture of misery so dire, that while you read, even your breasts will wince. The chapter devoted to breastfeeding begins with:
“Like everything to do with being a parent, don’t beat yourself up if you can’t feed your baby perfectly” (page 100).
So according to the author, Baird, only perfectionists breastfeed, which suggests that breastfeeding is perfection rather than a biological norm. This single opening sentence sets the defeatist tone for what is to follow:
“Although you need no extra calories to breastfeed, it is tiring and time-consuming in the first weeks of your baby’s life (not to mention rather painful)” (page 100).
“It is down to mum alone” (page 100).
Yes it’s down to mum alone – if she wants it that way, otherwise expressing is an option. Besides, even if it were down to mum alone, this is part of parenting. As parents, we often need to take on different roles, sometimes out of financial necessity, sometimes out of personal preference, and sometimes (like breastfeeding) out of biological stipulation. Convenience and parenting seldom go hand in hand. A book is doing its readers a great disservice if it suggests otherwise.
Other things that often don’t go hand in hand include this book - and accurate information. Page 102 states:
 |
| Like men's underpants that enhance the size of their crotch, the back cover of this book is appealing but the contents don't live up. |
I approve of deterring a dogmatic adherence to weight charts, however I also approve of correct information. Breastfed babies actually gain weight faster initially, then slow down around the 1-2 month mark (see, 'Timeline of a Breastfed Baby').
Another misunderstanding Baird seems to have is the belief that breasts are somehow shameful and embarrassing. Take this comment from page 101 for example:
“To avoid an upsetting situation when breastfeeding is newish, or if your child is a breastfeeding toddler, take the easy option and feed in out-of-the-way-spots”.
'To avoid an upsetting situation' for who exactly? Woe betide anyone should have to see a baby or (gasp) a toddler nursing – people might start to think that breastfeeding is normal. Here, Baird is contributing to an ‘out of sight, out of mind’ mentality. This ignorant attitude is projected throughout the book; for instance, page 102 advises mothers:
“If you plan to breastfeed for months rather than weeks then from an early age refer to your milk as mummy’s milk or num nums or use another language (lait, leche, susu) to prevent embarrassment when your inhibition-free toddler starts demanding tit or booby”.
This ‘suggestion’ is evidence of, and feeds into, a distorted view of breasts. It suggests that breasts are embarrassing when they are used for their primary biological purpose. It even suggests that breasts shouldn't be referred to by their true name in a breastfeeding context. Such an unhealthy, attitude towards the female body is also evident on the same page where Baird recommends that:
“Toddlers like to fiddle. If that usually means stroking your hair or your other breast you can distract them with a toy or nursing bead necklace”.
I shuck my head in dismay reading that. The message is: when your child attempts to initiate physical contact, you must deter them. I find this sad. Sending signals to a young child that stroking hair, etc is wrong can discourage them from future acts of tenderness. Breastfeeding is a tender act. It provides more to mother and child than simply a nutritive exchange. However our society is reluctant to recognise this side of breastfeeding. This is the same society that hyper-sexualises breasts, and does not provide support to enable mothers to achieve their breastfeeding goals. Baird seems determined to maintain this status quo. Page 102 maintains:
“If your partner or office has a time limit of tolerance it is fine to wean your baby. You’ve done a great job”.
No effort is made to suggest that the partner or office is unreasonable in their lack of tolerance. It is clear that Baird has a piecemeal approach to activism. On one hand, she wants to change society from a capitalist, environmentally-damaging social-order; yet on the other hand, she refuses to challenge the exact mechanisms which keep this order in place - the stringent employer who refuses to accommodate a mother’s right to feed her infant naturally. In this scenario, the mother will be nudged into formula feeding, and consequently, add to the regrettable impact on the environment this feeding method entails (see here). The anti-breastfeeding sentiment in this book is at stringent odds with its eco-friendly mission. Which leads us to the fifth and final exhibit for today...
Trade Secrets: Parenting
Annie Ashworth, Meg Sanders, and Karen Dolby
This is an ambitious book. Despite claiming to cover “everything you will ever need to know from conception to leaving home”, the book isn't the ton weight you would expect; in fact, it's relatively thin. So this must mean that the authors have consolidated all the most relevant and useful information, right?
[You know that farting buzzer sound you hear on game-shows to signal failure? Well, that would be appropriate here.]
The book begins with a list of “Things you’ll wish you hadn’t said during pregnancy”, at the top of which is: “I’m certainly going to breastfeed” (page 5).
Here, we see the defeatist attitude so common in pregnancy-related texts. This pessimism does not empower women. Instead it leads them to doubt themselves before they’ve even given birth.
From birth to the postnatal recovery period, the book moves swiftly from pessimism to martyrdom. In the “birth to six months” chapter, it advises new mums to:
“Try to be practical. If your partner is working during the week, let him sleep at night, even if this means using a spare bed during the week. It’s pointless having both of you exhausted and if you’re breastfeeding there’s little he can do to really help” (page 31).
So much for fathers facilitating breastfeeding via emotional and practical support! Nope, instead the authors prescribe that mum takes herself away to the spare bedroom, so her hubby can get a good night’s sleep. I can hear the 1950s calling.
But wait! Later, when dealing with older babies, the authors suggest:
“If weaning from the night feeds is difficult, try sleeping in a separate room from your baby and leave your partner to deal with the night feeds and changes” (page 73).
Contradictory some? One minute we're advised to let our partners sleep, then we're told to make them do the feeds and changes! So let me get this right, giving our partners free-reign sleep was only for the newborn days? (Y'know the initial period where mum is exhausted after just given birth). Then, our partner should do the night feeds, and as we're talking about babies here, that would mean either formula or expressed breast milk. The latter would require use of a breast pump, so presumably the authors know all about breast pumps.
“If you’re worried that you’re not producing enough milk, try using a breast pump” (page 36).
*sigh* Evidently not. Refer above to my comments regarding breast pumps and their impotence as measuring machines. It seems this book is falling into the same myths and boobie traps as all the others. Case in point:
“Offer solid food before you breastfeed” (page 42).
No. Please don’t do this. It will displace your baby’s desire for breast milk, which as I said above, is richer in nutrition. On the topic of nutrition and taste, the book seems confused:
“Some breastfed babies never really get used to the taste of cow’s milk” (page 103).
This random comment is not backed up with reasoning or evidence. There’s no reason why a breastfed child would be any more intolerant to cow’s milk than a formula fed child. More random nonsensical advice is given in regard to the issue of nipple-care:
 |
| Cabbage Couture - this book's idea of a good time (image from page 37). |
No. No. and NO. You know those little goose bumps on your areola? They secrete a natural oil which helps to lubricate your nipples and keep them in good working order. If you wash your breasts frequently, you will wash away this valuable oil. This will lead to more, not less, discomfort.
If you're still reading the book by this point, you are now presented with a list (yes another list! The lazy-ass authors love lists) titled “Looking After Yourself While Breastfeeding”. This figuratively translates to: ‘A List of Unnecessary Hurdles to Breastfeeding’. It features such gems as:
“Breastfeeding can leave you dehydrated and unable to produce enough milk. Aim to drink a pint of water before and during a feed” (page 38).
“What you eat effects your milk. Eat a sensible balanced diet. Avoid spicy food, oranges or too many citrus fruits” (page 38).
“Don’t eat nuts” (page 39).
“What you eat at lunchtime provides the milk for the evening feeds – so eat! Plenty of protein, calcium, carbohydrates, fruit and vegetables – and lots and lots to drink” (page 39).
“To keep up your milk supply, try to rest in the afternoon. That way you should still be producing plenty of milk for the evening feeds, and so have more chance of ensuring a settled night’s sleep” (page 39).
So basically the message here is, if you don’t have the diet of an athlete, you’d better pray for your breastfeeding relationship. Also you must remove any traces of substances that could possibly give taste to your food; drink like a camel; and somehow get rest every afternoon. Yup - regular REST! The authors of this book need to be sectioned, or at least forced to spend 48 hours with a newborn. Rest indeed. Pah!
But wait, there’s more:
“It’s better to completely empty one side in a feed” (page 35).
 |
| (Image from page 63) |
On the topic of demand, what if your baby demands a feed in public? (As they tend to do, inconsiderate little cherubs). Of course, the book has advice for this scenario too:
“For discreet breastfeeding in public, don’t wear dresses and avoid wearing anything that opens from the top downwards” (page 39).
You heard ladies; don’t button downwards - heaven forefend anyone get a flash of your top boob. (Surely in that case, we must ban most Topshop stock?) Not only is it unacceptable to publicly exposing even an inch of breast, this book also buckles at the mere mention of the word boob:
“If you’re breastfeeding your toddler by the time she can talk, be prepared for her to demand a feed, at the top of her voice, in the most embarrassing terms and in the most crowded place imaginable. This can be a major incentive to weaning” (page 73).
Here, we see the discourse of forced-weaning displayed in the oh-so-common parent-centric hierarchy of: parental convenience > parental comfort > comfort of strangers > child's needs (in that order). The desires of the parent and the public are placed miles ahead of the needs of the child. This approach is echoed earlier in the book with regard to young babies:
“It’s useful to get breastfed babies used to taking a bottle so that you are not their only source of food” (page 40).
There’s no mention of the (very real) risk of nipple confusion here; and no suggestion of waiting until breastfeeding is established before introducing a bottle. More to the point, is there anything inherently wrong with mum being a baby’s only source of food for 6 short months? Do we buckle when mothers are the only source of food for 9 months in utero? This book's emphasis on detachment parenting is illustrative of a major wrong in our contemporary society - parents want to enjoy the evolutionary immortality of having children without investing (what they perceive to be) the hard work, and so, turn to the bottle.
On the topic of bottle feeding, the book insists that:
 |
| (Image from page 74). |
So here, the authors are maintaining that formula provides a baby with ‘everything’ they need; that formula is not an inferior product. However on the packaging, commercials and marketing material even formula companies openly acknowledge that their product is inferior. The antibodies and brain building nutrients found abundantly in breast milk have naturally evolved to fulfil a biological need (see for example, “The Virgin Gut: A Note For Parents”). When she reads this book, an undecided mum-to-be is receiving a not-so-gentle nudge in the direction of formula feeding. After all, why endure the apparent diet restrictions, clothing restrictions, public embarrassment, crippling thirst, and lonely midnight breastfeeds, if formula is on par with breast milk?
Considering the book’s agenda of framing breast milk and formula as equal, it comes as little surprise when the scripted ‘top up’ discourse pops up on cue:
“Bottle-fed babies sleep through the night earlier than their breastfed contemporaries. This may be because many women’s supply of breast milk is reduced in the evening, often because of tiredness. Even if you are breastfeeding, topping up with a bottle can be a way to encourage your baby to sleep a bit longer” (page 41).
This paragraph is like a game of Boobie Trap Bingo: Bottle feeding parents get more sleep myth – check! Targeting mothers’ worries about supply – check! Tiredness diminishing supply myth – check! Recommending topping up without mentioning the risks – check! Putting parental convenience above infant need – check!
Supplementing breast milk with formula, as the book suggests, short-circuits the whole supply and demand process so central to successful breastfeeding. Take note: anything that reduces your baby's hunger or her need to suck will ultimately reduce your milk supply.
That nudge to formula feeding I was talking about before? Well that nudge becomes a ruddy big push on page 69, when the book looks at teething:
“If you are breastfeeding a teething baby, keep your little finger ready to lever her jaws apart. A teething baby can draw blood!”
This conjures imagery that would win Oscars in the Saw movies. The reality however is not as theatrical. In fact, it’s physically impossible for baby to nurse and bite at the same time, because the tongue covers the bottom teeth when baby is nursing. A baby may try biting before or after a feed as a playful experiment but this usually lasts only a few days once mum issues a stern ‘no’. Biting is not a sign of needing to wean, contrary to what the book then maintains:
“A baby who bites often while breastfeeding may be trying to tell you that she doesn’t need it anymore. Try just cuddling her instead and see how she reacts” (page 73).
As some babies are born with teeth, the assertion that biting signals a need to cease breastfeeding is nonsensical advice at best, and at worst - down right scary. Alas, the outdated yet persistently-popular equation of teeth with cessation of nursing is an example of how the book pushes parents to wean before the child is ready. Another example of the push to premature weaning can be found on page 80; as with so many anti-breastfeeding texts, it exploits parents’ desire for sleep:
“It is quite normal for a breastfeeding toddler to wake any number of times to nurse each night. Children who haven’t been breastfed or are weaned earlier may have soothers, blankets or toys to comfort them, instead of your breasts”.
There’s no reason why a child of toddler age cannot breastfeed through the day and use comfort objects at night.
Perhaps we shouldn't be surprised at the overwhelming parent-centric approach adopted in this book. After all, the authors' suggested antidote to an impending toddler tantrum is to suddenly slam a door, thus scaring the child (page 91). This makes as much sense as pumping to measure your milk supply, OCD washing of nipples, drinking your bodyweight in Evian, topping up, forced-weaning, and many of the other hurdles this book instructs mothers to fence.
So there you have it, five more anti-breastfeeding books. Suffice to say these should be pulped and recycled to save some of the world's trees. Alas, these are merely a few turds floating atop a huge cesspit of childcare manuals. You don't have to look farther than your local library, to find shelves lined with authors hell bent on sabotaging the already threatened art of breastfeeding. Do you know of a book I need to expose? Comment bellow.
↧
Boobie Trap Bingo
Pull up a chair and play a game of Boobie Trap Bingo with me! Which of the following have you overcome?
Why not open the bingo card in paint, and then circle the boobie traps you have overcome. Now you can display your bingo card on your Facebook profile, blog or Pinterest page! Many people assume that when a woman breastfeeds for longer than a few weeks, she 'must have had it easy'. For most breastfeeding mothers however, this is NOT the case. So why not let everyone see how strong you are.
↧
↧
Triumphant Tuesday: Breastfeeding Triplets!
What's triumphant about Tuesdays, you may be pondering? Well, Tuesdays are now THE day of the week to celebrate success in infant feeding (Friday's are SO cliched! Yawn).
It all started with a post I made on Facebook. Turns out, this post had mothers spitting and snarling at each other like a bunch of dogs fighting over a bitch. Here's my post:
"Calling all breastfeeding moms!! You may be aware of a certain blog where formula feeders drone on about their story of hardship, about the boobie traps which snared them, the breasts which failed them. Every Friday there is a new tale of woe. Welllllll... how about we make our own - but with a positive twist! I'm going to put together a collection of stories from breastfeeding moms who have OVERCAME boobie traps, using their hard work and determination. Whether the hurdle was postnatal depression, mastitis, unsupportive family members, low supply, or anything in between. Did YOU have a challenging breastfeeding experience? Get typing and email me at thealphaparent@gmail.com I will showcase your story on the blog!"
It all started with a post I made on Facebook. Turns out, this post had mothers spitting and snarling at each other like a bunch of dogs fighting over a bitch. Here's my post:
"Calling all breastfeeding moms!! You may be aware of a certain blog where formula feeders drone on about their story of hardship, about the boobie traps which snared them, the breasts which failed them. Every Friday there is a new tale of woe. Welllllll... how about we make our own - but with a positive twist! I'm going to put together a collection of stories from breastfeeding moms who have OVERCAME boobie traps, using their hard work and determination. Whether the hurdle was postnatal depression, mastitis, unsupportive family members, low supply, or anything in between. Did YOU have a challenging breastfeeding experience? Get typing and email me at thealphaparent@gmail.com I will showcase your story on the blog!"
...And so we have the first ever Triumphant Tuesday! Every week I will post a story of a truly fearless breastfeeding mom. This week's story defines fearless!
Two breasts. Three babies. It doesn’t look like Mother Nature did the math on this one. Yet even the seemingly impossible wasn’t enough to deter this mom from giving her babies the natural start they deserved.
Two breasts. Three babies. It doesn’t look like Mother Nature did the math on this one. Yet even the seemingly impossible wasn’t enough to deter this mom from giving her babies the natural start they deserved.
Let me introduce Davina. She endured inverted nipples, cracked nipples, and an unsupportive husband. Then... nature dished out its biggest challenge.
This is her story.
"My first child, a baby girl, was born two decades ago. I was 21 and went home with her after a week in hospital with very little ongoing support or advice. My first memory of breastfeeding was a nurse just grabbing my breast (without asking) and shoving it in her mouth. My nipples were completely inverted prior to breastfeeding. No-one ever told me this could be a problem. My mom was open about how she only breastfed me and my sisters for 6 weeks each, and I was the first to produce grandchildren so I had no breastfeeding role models. I just got on with it really.
Nipples Hanging on by a Thread
After a few weeks my nipples were badly cracked. The damage was so severe that one side looked about ready to fall off. At the time, I didn’t know what the pain was and just carried on until the nipple was literally hanging by a thread! I had no knowledge of correct latch. I thought babies just ‘got it right’ through instinct. I tried nipple shields but found them cumbersome and pretty useless.
I never thought of giving up breastfeeding. Instead, I called La Leche League who sent someone out to check what was going wrong. They helped me, and I expressed milk and fed my daughter with a bottle for a couple of weeks until my nipples had healed - then I was right back at it!
I went on to breastfeed my daughter for 13 months when she self-weaned probably due to me getting pregnant with my second daughter. I breastfed her also for 13 months, when she also self-weaned. By this time, my nipples were no longer inverted and have never gone back to that shape ... which is a blessing considering what was going to happen!
The Birth of the Triplets
| Triplet Cuddle! |
The biggest challenge to my breastfeeding journey came 20 years later when I gave birth at 41, to triplets. They were born early at 34 weeks. Consequently, they had to learn how to feed as the suck/swallow/breathe action required for feeding doesn’t normally kick in until about 35/36 weeks.
Unsupportive Medical Staff
Again, I never thought for a minute that I wouldn’t be able to breastfeed my babies. However sadly, no one shared my confidence. Everyone told me it would be impossible...midwives, nurses, specialist doctors... even though the hospital actively encouraged breastfeeding - apparently this didn’t apply to triplets. The medical staff would nod and smile in a patronizing manner when I said I would be breastfeeding the triplets. They even told me I should ‘practice’ with formula before I took the babies home so that I wouldn’t have to learn it when I was completely frazzled by them screaming because they were starving! No one ever made any positive comments about my decision to breastfeed. Not one. Even the Lactation Consultant, who came round the NICU, wasn’t encouraging. She was just ‘good on you for trying’, but not saying ‘you can totally do this, here’s some info on bf triplets and the number for LLL and some other women who have done it’.
Unsupportive Husband
My husband, being a first time dad, was very much ‘doctors are God, and if they say we should practice with bottles, then we should’. I often had to say to him, ‘yes I am very tired, but I am not supplementing with formula just to get some sleep, or so your mother can ‘help’. I am breastfeeding and that’s that.’
Growth Spurts and Sleep Deprivation
Of course, I ignored the formula-pushers, and by the end of the third week in NICU my babies were home. I have always been blessed with a great milk supply, or maybe it’s just a normal milk supply and I am blessed with great confidence in my body’s ability. Nonetheless, that doesn’t mean it was easy. Growth spurts were hard work when I literally didn’t do anything except feed, feed, feed. Complete sleep deprivation has been a major issue because I am the only food source. My husband and I had to work out a strategy for us to both to get some sleep. After some trial and error we settled on the following routine:
- I breastfeed all babies all day
- I breastfeed our son all night
- I pump about 400ml of breastmilk first thing in the morning
- My husband feeds the girls this EBM during the following night
During the night, co-sleeping was a life-saver! During the day, each baby needed only one side for a full feed, and even if they feed one after the other there is usually enough for everyone and if not, then the one who feeds last might get what’s left in both sides.
The triplets are now nearly 10 months old and all weigh over 8kg, (18lb) so mama’s milk is some gooood stuff!
Women Who Don’t Breastfeed
I am very judgemental about women who don’t even try to breastfeed. I kinda wish I wasn’t, but I can’t help it. Women who try their best and it doesn’t work, ok. However, women who give it a half hearted go and then blame low milk supply or something - I don’t have a lot of time for them. There is soooo much information and support and education and other moms to talk to, I just don’t get how mother nature could’ve gotten it so wrong, that so many mothers ‘can’t’ breastfeed. I don’t believe it.
I think that through inverted nipples, cracked nipples and multiple babies the thing that stands out to me wasn’t luck, or even support and role models, because I never really had those...it was just a confidence in myself, a belief that my body could do it, if I would just trust it. When my babies were feeding constantly my first thought wasn’t ‘I don’t have enough milk’, it was ‘growth spurt’...When they were spilly I didn’t think ‘I must have eaten the wrong thing’, I thought ‘prem babies have immature throat/tummy sphincters’...When they were grizzly my first thought wasn’t ‘what am I doing wrong’, it was ‘teething’...I’ve seen obstacles as external issues that can be controlled or passed through, not as something internal like my body is failing me. I believe this is key...all the support in the world won’t help until women give themselves some confidence, faith, trust, and belief.
The only challenges I have now are sleep deprivation, and people starting to say that because my babies are nearly 1, it’s time to wean. However I see this as my full time job. Sure, breastfeeding takes up a lot of time, but it’s my commitment to my babies."
Davina’s Bingo Card:
↧
Triumphant Tuesday: Breastfeeding and Homeless
It's often said that formula feeding is only unsafe in undeveloped countries where there is poverty and poor sanitation. This is a fictitious claim circulated by defensive formula feeders in an effort to justify their choice.
As we’ve learned over the past couple of years, disaster can strike anyone, anywhere and anytime. It doesn’t matter whether you live in a rich capitalist nation, or one that is poverty-stricken. A natural disaster, whether hurricane, tornado, flood, or tsunami, can devastate areas and leave families without resources, sometimes for long periods of time. In these instances, breastfeeding is a life-preserver.
The star of this week’s Triumphant Tuesday is Kate. When a flood destroyed her home, Kate lost everything. This tragedy pushed her into deep depression. Yet she was determined that her breastfeeding relationship would not suffer.
“When I became pregnant with my daughter I had the no-plan plan because I am the most indecisive person ever. All I did know was that I wanted a healthy happy baby. Then, early on in my pregnancy I took a nasty fall. I sprained my back and neck with a lot of other injuries.
A Complicated Pregnancy
The worst feeling is being told that we would have to "wait and see" if my daughter would be affected by the medication that was given to me by the hospital - the same hospital that knew I was pregnant!! I had such a painful pregnancy; And it didn't make it any easier that I wasn't given the comfort of knowing whether my baby would be healthy or not.
Later in my pregnancy the doctors believed I was on the verge of becoming preeclamptic due to abnormal test results. So everyday they were running tests on me. Nothing was making sense to them.
The Flood
In the midst of all of this my home was destroyed in a flood. We lost everything. All of a sudden there were so many unknowns. My home became a motel room and just the very thought that I would have to bring my newborn (that may not even be healthy) to this place sent me into periods where I would sob for hours. I felt incredibly guilty because now my daughter didn't have a house to grow up in, let alone her own room! Unsurprisingly I spiralled into deep depression, before she was even born.
An induction date was set, yet still I had no definite plans for labor or feeding. I decided I was going to try my best and see where labor took me, rather than trying to control it.
After my beautiful baby girl arrived I put her to the breast and just kept thinking, "If it hurts she isn't latched right". So if it hurt I would unlatch her and try again. She was born at 6 lbs 11 oz and at 3 days old she was already 7 lbs 1 oz and ABSOLUTELY HEALTHY.
Unhealthy Thoughts
As a consequence of my very stressful pregnancy and my existing depression, I developed postpartum depression. I was expecting to feel this overpowering love for my daughter. I thought I should feel so happy but all I could do was cry and all I wanted to do is sleep. I felt overwhelmed by the world around me and had daily panic attacks. It was as if an engulfing pain would course through my body, my chest would tighten, and I wouldn't be able to breathe.
To make matters worse, at the time we brought her 'home' from the hospital, her Dad was working over 12 hours a day, 6 days a week just to keep the roof over our heads. The time he was home he spent sleeping.
I felt like everyone was passing judgement onto me for living in a motel. People would suggest that I could have prevented ending up there. It made me feel like I had done something wrong, not that a flood took my home and my belongings.
During this time I was convinced something bad was going to happen to my baby. I couldn't sleep because when I did, someone or something was always hurting her. Once I started having scary thoughts about harming myself because I believed that I wasn't worthy of life. During that time, my daughter is what kept me on this earth. The closeness that we built while breastfeeding is something that no medicine or therapy could ever replicate.
![]() When I would try to talk to my doctors or nurses about my depression, they kept saying to me, "oh yes, having a newborn can be so overwhelming". That just made me want to scream more, because my newborn was the only thing holding me together. My emotions were just out of control but my little Sophia brought me back to me being me. She gave me focus. Every month that passed and I was still nursing, was something I could be proud of.
When I would try to talk to my doctors or nurses about my depression, they kept saying to me, "oh yes, having a newborn can be so overwhelming". That just made me want to scream more, because my newborn was the only thing holding me together. My emotions were just out of control but my little Sophia brought me back to me being me. She gave me focus. Every month that passed and I was still nursing, was something I could be proud of.
'Breastfeeding Snob'
These days I can honestly say I am somewhat of a breastfeeding snob. When I talk to pregnant ladies who aren't even considering breastfeeding because it's "weird" or they just don’t like the idea of it, I rattle off my long list of why they should! A part of me even looks down on people who don’t make an honest attempt at breastfeeding. I think, "Don't they know the benefits not only for their baby but for themselves as well?" Sometimes I feel like people just don't try hard enough. Parenting was not meant to be easy. Every pregnancy, child and mother is different but one thing is for certain - there is only one way that you SHOULD feed your child and if you don't make a whole hearted attempt at it for YOUR BABY then you really shouldn't be a parent.
My daughter is now 6 months old and has been exclusively breastfed, even when I myself wasn't able to get out of bed. She NEEDED me, so I was there for her. It’s as simple as that.”
Get your own Bingo Card here.
Email me with your story.
As we’ve learned over the past couple of years, disaster can strike anyone, anywhere and anytime. It doesn’t matter whether you live in a rich capitalist nation, or one that is poverty-stricken. A natural disaster, whether hurricane, tornado, flood, or tsunami, can devastate areas and leave families without resources, sometimes for long periods of time. In these instances, breastfeeding is a life-preserver.
The star of this week’s Triumphant Tuesday is Kate. When a flood destroyed her home, Kate lost everything. This tragedy pushed her into deep depression. Yet she was determined that her breastfeeding relationship would not suffer.
“When I became pregnant with my daughter I had the no-plan plan because I am the most indecisive person ever. All I did know was that I wanted a healthy happy baby. Then, early on in my pregnancy I took a nasty fall. I sprained my back and neck with a lot of other injuries.
A Complicated Pregnancy
The worst feeling is being told that we would have to "wait and see" if my daughter would be affected by the medication that was given to me by the hospital - the same hospital that knew I was pregnant!! I had such a painful pregnancy; And it didn't make it any easier that I wasn't given the comfort of knowing whether my baby would be healthy or not.
Later in my pregnancy the doctors believed I was on the verge of becoming preeclamptic due to abnormal test results. So everyday they were running tests on me. Nothing was making sense to them.
The Flood
In the midst of all of this my home was destroyed in a flood. We lost everything. All of a sudden there were so many unknowns. My home became a motel room and just the very thought that I would have to bring my newborn (that may not even be healthy) to this place sent me into periods where I would sob for hours. I felt incredibly guilty because now my daughter didn't have a house to grow up in, let alone her own room! Unsurprisingly I spiralled into deep depression, before she was even born.
 |
| Kate's porch. This picture was taken before they were evacuated. The water was already coming up to the door of the house, despite the porch being elevated 4 steps from the ground. |
An induction date was set, yet still I had no definite plans for labor or feeding. I decided I was going to try my best and see where labor took me, rather than trying to control it.
 |
| Little Sophia is born. |
Unhealthy Thoughts
As a consequence of my very stressful pregnancy and my existing depression, I developed postpartum depression. I was expecting to feel this overpowering love for my daughter. I thought I should feel so happy but all I could do was cry and all I wanted to do is sleep. I felt overwhelmed by the world around me and had daily panic attacks. It was as if an engulfing pain would course through my body, my chest would tighten, and I wouldn't be able to breathe.
 |
| Their first family photo. |
I felt like everyone was passing judgement onto me for living in a motel. People would suggest that I could have prevented ending up there. It made me feel like I had done something wrong, not that a flood took my home and my belongings.
During this time I was convinced something bad was going to happen to my baby. I couldn't sleep because when I did, someone or something was always hurting her. Once I started having scary thoughts about harming myself because I believed that I wasn't worthy of life. During that time, my daughter is what kept me on this earth. The closeness that we built while breastfeeding is something that no medicine or therapy could ever replicate.
 When I would try to talk to my doctors or nurses about my depression, they kept saying to me, "oh yes, having a newborn can be so overwhelming". That just made me want to scream more, because my newborn was the only thing holding me together. My emotions were just out of control but my little Sophia brought me back to me being me. She gave me focus. Every month that passed and I was still nursing, was something I could be proud of.
When I would try to talk to my doctors or nurses about my depression, they kept saying to me, "oh yes, having a newborn can be so overwhelming". That just made me want to scream more, because my newborn was the only thing holding me together. My emotions were just out of control but my little Sophia brought me back to me being me. She gave me focus. Every month that passed and I was still nursing, was something I could be proud of.'Breastfeeding Snob'
These days I can honestly say I am somewhat of a breastfeeding snob. When I talk to pregnant ladies who aren't even considering breastfeeding because it's "weird" or they just don’t like the idea of it, I rattle off my long list of why they should! A part of me even looks down on people who don’t make an honest attempt at breastfeeding. I think, "Don't they know the benefits not only for their baby but for themselves as well?" Sometimes I feel like people just don't try hard enough. Parenting was not meant to be easy. Every pregnancy, child and mother is different but one thing is for certain - there is only one way that you SHOULD feed your child and if you don't make a whole hearted attempt at it for YOUR BABY then you really shouldn't be a parent.
My daughter is now 6 months old and has been exclusively breastfed, even when I myself wasn't able to get out of bed. She NEEDED me, so I was there for her. It’s as simple as that.”
Kate's Bingo Card:
Email me with your story.
↧
So You’ve Given Up Breastfeeding...
I often have to sit and listen to assorted tales of woe from women who gave up breastfeeding because they had mastitis, cracked nipples, a c-section, the runs.
It seems that a large proportion of formula feeders are not happy with their choice. Statistics back this up: “Every year more than 200,000 mothers stop breastfeeding in the first few days and weeks – 90% of these mothers would have liked to continue” (The Guardian 2011).
It seems that a large proportion of formula feeders are not happy with their choice. Statistics back this up: “Every year more than 200,000 mothers stop breastfeeding in the first few days and weeks – 90% of these mothers would have liked to continue” (The Guardian 2011).
Now of course, these women will swear blind that they did not give up breastfeeding due to lack of effort. Great! Because what I am about to suggest will require effort in spades
- Relactation!
It’s never too late to breastfeed. Breast milk is a flexible resource. Amazingly, it’s also possible to induce lactation when you’ve never given birth or ever been pregnant. So there really is no excuse ladies! Here’s how it’s done:
You’ll need to pump every two to four hours, day and night. Some women start to produce milk within three weeks, while others may need six weeks or more. If you’re relactating, the rule of thumb states that it will take at least the same amount of time to begin lactating as has passed since you weaned, so if it’s been six weeks since you breastfed, it will probably take six weeks to fully lactate.
Try not to become discouraged if you have little or no visible milk production while pumping. There's something about a real baby, her smell or the feel of her in your arms, that jump-starts lactation like nothing else. Close your eyes while pumping and think about your little one. Creative visualization can affect your whole body.
Try not to become discouraged if you have little or no visible milk production while pumping. There's something about a real baby, her smell or the feel of her in your arms, that jump-starts lactation like nothing else. Close your eyes while pumping and think about your little one. Creative visualization can affect your whole body.
Here’s my four-step feeding process for relactating:
1. If possible, breastfeed for a few minutes to encourage the baby to associate the breast with feeding. Provide skin-to-skin contact.
2. Supplement the feeding with a supplemental feeding device (such as THIS one) that can be used while baby nurses.
3. Cut out any other source of sucking; This includes a pacifier.
4. Pump using a high quality breast-pump (Look for one that provides an automatic suction-release cycle that mimics your baby's suck; THIS is the best one - these hospital-grade pumps offer double pumping, are great for establishing a strong milk supply, and are perfect for the working mother).
Regarding step 2: initially you will need to carry on feeding your baby with formula until your milk supply has got going again. This is where the supplemental feeding device (SFD) comes in. A SFD is a device whereby your baby sucks formula from a small tube taped to your nipple, thus stimulating your milk production as he sucks.
When the time comes to put your baby to the breast, you have to be patient. Many older babies are often a little reluctant to nurse from a breast at first, as they’ve been bottle fed and may need time to become accustomed to the breast.
Think positive: you can build up a milk supply once more. If adoptive mothers can do it, so can you!
↧
Triumphant Tuesday: Menacing Medical Staff
 Formula-peddling. A beloved pastime of many medical staff. You see, formula enables doctors, nurses and other assorted white-coats to escape the responsibility of actually *solving* a breastfeeding problem. Handy, no? It also masks the fact that these ‘professionals’ don't have breastfeeding-related training stretching beyond flicking through a Cow & Gate brochure. Consequently they can’t tell a latch-on from a let-down. By manipulating exhausted and scared new mothers into formula feeding, medical personnel can tick the box on their chart for ‘weight gain’ and send the mother on her way. Next!
Formula-peddling. A beloved pastime of many medical staff. You see, formula enables doctors, nurses and other assorted white-coats to escape the responsibility of actually *solving* a breastfeeding problem. Handy, no? It also masks the fact that these ‘professionals’ don't have breastfeeding-related training stretching beyond flicking through a Cow & Gate brochure. Consequently they can’t tell a latch-on from a let-down. By manipulating exhausted and scared new mothers into formula feeding, medical personnel can tick the box on their chart for ‘weight gain’ and send the mother on her way. Next!So many mothers succumb to this approach, which often borders on bullying. Like school yard bullies, medical staff have years of manipulation experience, an arsenal of verbal and psychological weaponry, and an army of allied peers. They target the most vulnerable and use their disproportionate power to overwhelm their victim. It takes a truly fearless woman to stand up to these tyrants - Molly is one such woman.
“Going into this pregnancy I knew I wanted to breastfeed more than anything. My mother and two older sisters had done it and it seemed so easy and wonderful. I could not wait to share that bonding experience with my baby as well. My family were on board and I thought that it was going to be no problem. I read lots of articles on breastfeeding and even read up on boobie-traps before I went into labor. What could possibly go wrong?
I was in labor for almost 24 hours when my daughter, Kyla finally arrived. She was what they were calling "cheesy". This means she swallowed some gunk on the way through the birth canal and some of it got down in her lungs. The nurses wanted to take Kyla from me as soon as she was born. Luckily I had my older sister there who had breastfed both of her kids and she begged them to just give me one minute of skin on skin contact. They agreed and gave me my one minute.
When they brought Kyla back to me three hours later, she was starving. So, with my sister’s help, we latched on Kyla and she nursed for 30 minutes. The rest of the day was about the same. Kyla would nurse for a while and was doing just fine.
However the next day was a different story. For some reason my nipples were not cooperating, they were almost inverted; consequently Kyla was not latching well. She was also very exhausted. We would try to work on nursing for a while but she would just fall asleep. I felt confused since she had latched so well before. I phoned the lactation consultant. She described different techniques but told me not to worry, that babies are born with a lot of calories on board and Kyla was probably just very exhausted from the birth.
Now my husband is a stickler for following the rules so when the nurses gave us the chart where we had to write down every time she ate, peed, or pooped, he follow directions adamantly. This ended up being our downfall. Every time I asked for assistance I would get a different nurse. None of them were very helpful. One of them even said, "Something is wrong with you; that's why she's not latching on. She's probably going to have to have formula because something is going on with your nipples."
Later, one nurse came in and saw how little Kyla had been eating based off the chart my husband had been filling out. The nurse started giving me a hard time. She said she's going to check my daughter’s blood sugar and that if it was below 40, it was the hospital's policy that they HAD to give her a bottle of formula. I started crying and arguing with the nurse, and I demanded that the lactation consultant be called to my room.
They went ahead with the blood sugar test, pricking my poor baby's foot and the result was 65. Yet the nurses still insisted that since it'd been so many hours since she had a ‘good feeding’ they were going to give her a bottle of formula. She and the lactational specialist started to argue with each other on either side of me, with me crying in the middle trying to get my baby to nurse. My husband was whispering in my ear that he would not let them give Kyla a bottle of formula; that he would check us out of the hospital against doctors orders before he would let that happen to us. He kept lovingly reassuring me that everything was going to be okay and he would not let them do anything to our baby that we did not want [Alpha: 'Husband of the Year Award' anyone?]
While the arguing was still going on, all of a sudden my baby girl latched onto me and started eating. Everyone stopped talking and watched her nurse. The lactation consultant remarked, "See! She's doing it! She's fine; you're not going to give her a bottle of formula." The nurse stormed out of the room. Kyla nursed for a good 30 minutes during that feeding.
My husband kept filling out the chart, but he hid it whenever someone came in the room. That night when the nurses wanted to take Kyla so my husband and I could get some sleep, we were very reluctant to let her leave. It was a different nurse on duty, but still we were afraid of what they would do if Kyla was away from us. So my husband made a sign for her carrier that said, "NO formula please! If she cries bring her back to her momma."
The rest of the hospital stay was challenging because my nipples remained inverted for whatever reason. However, I continued to work with the lactation consultant who gave me some latch assistants. They looked like little turtle shells that you put on your nipples when you aren’t nursing, and the suction makes your nipples hard. They helped a little bit. The biggest thing that helped was time. After 2 weeks, my nipples went back to normal.
I am proud to report that I currently have a six-month-old baby who is still exclusively nursing. I'm so glad that I didn't listen to the nurses, and that I had faith in my baby and faith in my body. Breastfeeding is the best gift that I can give my child and I'm so happy that I am able to do it. I don't want any other mother to have to go through what I went through in the hospital. Thank God for good lactation consultants and for my husband and sister for their solidarity.
I really feel sorry for people who don't try breastfeeding. They are missing out on a truly spiritual, amazing, financially pleasing, bonding experience that I have ever had.”
Molly's Bingo Card:
Get your own Bingo Card here.
Email me with your story.
↧
↧
Triumphant Tuesday: Breastfeeding with Tongue-Tie
 Most of us think of tongue-tie as a situation we find ourselves in when we are too excited to speak. In fact, tongue-tie is the non-medical term for a relatively common physical condition that limits a baby's use of it's tongue – and, if left undiagnosed, can be the final nail in the coffin of your breastfeeding relationship. Tongue-tie occurs when the thin piece of skin under the baby's tongue (the lingual frenulum) is abnormally short and may restrict the movement of the tongue tip. This can interfere with the baby's ability to suckle efficiently at the breast, leading to nipple pain and trauma, poor breastmilk intake and a decrease in milk supply over time.
Most of us think of tongue-tie as a situation we find ourselves in when we are too excited to speak. In fact, tongue-tie is the non-medical term for a relatively common physical condition that limits a baby's use of it's tongue – and, if left undiagnosed, can be the final nail in the coffin of your breastfeeding relationship. Tongue-tie occurs when the thin piece of skin under the baby's tongue (the lingual frenulum) is abnormally short and may restrict the movement of the tongue tip. This can interfere with the baby's ability to suckle efficiently at the breast, leading to nipple pain and trauma, poor breastmilk intake and a decrease in milk supply over time.Diagnosis is only the first hurdle however. The decision to release a tongue-tie often depends on a doctor's personal belief about the possible impact on feeding. Currently, doctors are divided in opinion, which leads to a lottery of patchy treatment for breastfeeding mothers.
Emma drew the short straw in this lottery. Here is the story of her struggle to get her son’s tongue-tie taken seriously.
Sent to NICU
 |
| Samuel in NICU |
When Samuel was born, because there was meconium in the amniotic fluid, the pediatrician sent him to the NICU for monitoring and tests to check if he had an infection. Samuel was put on antibiotics as a precaution. As a result, he got thrush which took a while to clear up.
Samuel was born at 6:49pm, yet it wasn't until 3am the following morning he was released from the NICU and was allowed to breastfeed for the first time. I became so anxious about nursing him in the hospital that I couldn't get him to latch and needed the help of a midwife every time I wanted to feed him. That night he fed for an hour, sleep for an hour, then wake screaming for more. As a first-time mom I didn’t know this was normal newborn behaviour. In fact, the midwife told me to give him formula because I couldn't possibly keep up with him as he was so big. As she suggested formula I could feel my face falling. The midwife was polite, but in an overbearing, condescending sort of way. It seemed like she thought formula was much the same as breast milk. Up until that point I had been confident in my ability to feed my son. It felt as though everything had come crashing down. I was in tears. I knew giving formula would negatively impact my milk supply so I didn't. The midwife tried to help me manually express some colostrum, but as you'd expect we didn't get much and I was very stressed out at the time. My son was barely 24 hours old and I was already failing.
Once Samuel fell asleep, the midwife took my observations, and my pulse was through the roof (I think I was on the verge of a panic attack). She asked if I was in pain; I said I was stressed. She then gave me panadol to help me sleep. The next time my baby woke – I was so drugged up that I didn’t hear him.
Baby weight loss
By the time we left the hospital Samuel was had dropped from his birth weight of 4.424kg (9 pounds 12 ounces) down to 4.1kg. On the drive home I was bawling. I had tears streaming down my face. I cried through each feed for the rest of the day.
At his two week check he still hadn't regained his birth weight; in fact he had lost 45g. The only advice the health visitor offered was to top him up with formula. She even asked who my GP was, so she could keep tabs on me. This was my lowest day in a long time. I spent the rest of it in tears. I couldn't even feed my own baby. I had failed at being a mother.
After a phone call to the Australian Breastfeeding Association (ABA) I started to feel little better. I just kept feeding on demand (which was a lot). Samuel also had a handful of formula bottles when I knew he was hungry and I couldn't satisfy him.
At his 10 week check he only weighed 4.6kg. I was devastated. Things were not helped at times when my mother saw Samuel and she would regularly comment on how small he was. Every time I spoke to her she asked if he was still feeding as much.
Investigating the latch
I decided to ask a professional to check his latch, so we saw a lactation consultant at the hospital I gave birth in. I asked her specifically about tongue tie and lip tie and she told me he was fine and he just had a small mouth.
I had a feeling his tongue didn't look normal so later that day I called the ABA helpline and described his tongue. The counsellor told me I had described a tongue-tie perfectly.
I went to see our regular doctor about the tongue-tie. He told me that because Samuel could move his tongue somewhat, he was fine. My instincts told me otherwise.
Determined not to give up, I saw a THIRD professional; this time, a IBCLC who was able to direct me to a FOURTH professional – a laser dentist.
Samuel was 10 1/2 months when the tie was cut. I returned to work two days a week when he was 6 ½ months and negotiated to pump at work.
He is now 12 months and we are still breastfeeding. The unhelpful voices are still there: every time I talk to my mother she tells me he will wean in a month or two and she asks me whether I think he still feeds as much as he used to. When I see my doctor (the one who would not treat the tongue-tie) he tells me I should wean Samuel now that he is 1 year old. I have learnt to ignore such negativity.I plan on letting Samuel self wean. Needless to say I am in the market for a new doc; but I can't get a refund on my mother.
I really enjoy breastfeeding my little boy. I often think that, if instead of making me feel bad, the health visitor had suggested an IBCLC, I wouldn't have spent those precious first moments as a new mother worrying about my sons weight gain and feeling like I was a failure. When I look at photos he does look skinny; it breaks my heart to think he was hungry because no one suggested anything helpful, like an IBCLC.”
Emma's Bingo Card:
Get your own Bingo Card here.
Email me with your story.
↧
Triumphant Tuesday: Commercially-Motivated Medical Staff
 As I wrote in the article: '15 Tricks of Formula Companies', getting health professionals on side is a common strategy of formula companies. New mothers understandably carry the assumption that health professionals have significant expertise in the areas they counsel, and that health professionals always have the baby’s best interests at heart. However the reality is that a baby’s interests, and indeed a mother's interests, are often misplaced by commercial interests when a health professional has been corrupted by formula companies. Cera is a mother who experienced this first hand. When Cera became pregnant with twins, the sabotaging remarks of her family were the least of her worries...
As I wrote in the article: '15 Tricks of Formula Companies', getting health professionals on side is a common strategy of formula companies. New mothers understandably carry the assumption that health professionals have significant expertise in the areas they counsel, and that health professionals always have the baby’s best interests at heart. However the reality is that a baby’s interests, and indeed a mother's interests, are often misplaced by commercial interests when a health professional has been corrupted by formula companies. Cera is a mother who experienced this first hand. When Cera became pregnant with twins, the sabotaging remarks of her family were the least of her worries...“My name is Cera (pronounced Sarah). I am 22 years old and proud mom to beautiful twins. I was blessed to have a boy and a girl. They are happy, bouncy, smiling bundles of joy and my husband and I couldn't be happier. It however didn't start out that way...
Unsupportive Family
My family has a really bad tendency to tell me exactly how they feel at any given time, so when I was pregnant with twins and they found out I was going to attempt to breastfeed they had no problem telling me I was nuts! My mother in law informed me that breastfeeding was like a ball and chain, and that it was embarrassing to do anywhere but at home. She told me that she used formula with her youngest child because she didn't like to breastfeed. That in itself planted seeds of doubt in my psyche about breastfeeding.
The next big "confidence boost" came from my ever loving sister. She had a c-section with my niece and after a couple of failed nursing attempts, turned to formula. If anything I feel that she was jealous of my determination not only to breastfeed, but to feed two babies. She informed me that I wouldn't release any milk because I was not having a natural child birth. I wasn't convinced, so I bit my tongue and carried on. It wasn't until my third trimester when I woke up to a milk soaked bed did I realize that there was hope for me!
Skin-to-Skin Interrupted
On June 4th I was finally in hospital for my scheduled c-section to bring my twins into the world. I was 38 weeks pregnant and bigger than I ever thought a pregnant woman could get! After the babies were put into my arms, I was more than ready to start the bonding and beauty of breastfeeding. My husband stayed to help and watch as my little 6 pound babies were nestled under my arms and up to my breasts. After both babies successfully latched, I was ecstatic. I beamed with pride and relief and forgot about all of the grief I received from friends and family telling me there was no way with a c-section and twins, that I would never be able to breastfeed. With panic aside, I happily bonded with my husband and newborns. That was until the lactation specialist walked into the room.
She busted through the doors into my room and instantly started barking orders. I knew right away I wasn't going to enjoy the company of this woman. She saw my little baby boy sleeping sound, snuggled against me after he had just finished his meal. She then grabbed him from my hands to undress him, rub him and put an ice cold wash cloth on him. I was shocked to say the least. I fully understood that you have to wake your babies to get them to eat, but to interrupt my bonding time was more than appalling. After she put my son back onto my breast and move onto my daughter, I politely asked if my husband could try and wake her.
Two days later I was getting into the groove of breastfeeding. I thought all was well and I was in Mommy bliss! However one evening the lactation specialist came into my room with a scale to weigh the babies and 'make sure I was producing enough for them'. This is when we found out both of my babies had lost a significant amount of weight. I was mortified. I couldn't believe it. My baby bliss just melted away with one scorned look from this woman. She lectured me about not waking them up regularly enough (even though I woke them every 3 hours as I was instructed) and she accused me of not listening to her. A flood of tears hit me. I was alone in the room with her since my husband had left to get some clean clothes and feed our pets at home. When he walked back into the room he found me pale faced and bawling my eyes out. The thought that I could be starving my children made me sick.
With careful consideration, we asked one of our wonderful nurses to not allow that nasty woman back into our room. After a lot of prayers and help from the nurses, in a few days we got our babies weight back up and breastfeeding returned to a happy experience for everyone. Sadly, this harmony was short-lived. The next day the specialist came back into our room to apologize (even though I didn't want to hear it) and to proceed to tell me that if I didn't have a Medela Breast Pump that I was not leaving the hospital without buying one from her. I was livid! After all this woman had put me through, and now this?? I couldn't believe it! I told her that I had a nice brand new pump at home and she proceeded to tell me that it wasn't good enough. I was now captive!
With my mom at my side, we called every mother we knew and our insurance to try to get me a Medela. Finally an acquaintance of my husband’s friend had one that I could borrow and we got our babies home.
Now my babies are both growing healthy and happy with full tummies that I proudly provide. I constantly get compliments from other mothers and even doctors for not needing to supplement my two "not so little" ones. If I had the chance to speak to any young mothers of multiples that are hoping to breastfeed without supplement, I would tell them to never give up on what you feel is right for your babies. It will get easier in time.”
Cera's Bingo Card:
Get your own Bingo Card here.
Email me with your story.
↧
Babies Asleep in Walkers
Is there any sight cuter than a baby blissfully dozing in dreamland? YES! A baby blissfully dozing in dreamland IN A WALKER!!
When I found my son doing it, I wondered whether this was a common phenomena. So I enquired on The Alpha Parent Facebook group. The result? Welcome to the...
'Babies Asleep in Walkers Hall of Fame!'
Do you have a photo of your sleeping cherub in a walker, jumparoo, bouncer, or activity center? Do you have a sense of humour? If so, email me and you could star in the Hall of Fame!
When I found my son doing it, I wondered whether this was a common phenomena. So I enquired on The Alpha Parent Facebook group. The result? Welcome to the...
'Babies Asleep in Walkers Hall of Fame!'
Neil:
Cameron:
Brynn:
Clyde:
Morgan:
Anon:
Anon:
Jaxton:
Anon:
Anon:
Jaycee:
Jaycee again
She's a veteran sleep-walker (see what I did there?)
Ethan:
Kyla:
Azure:
Sofia:
Anon:
Isabel:
Elija:
Harlow:
Ender:
Fergus:
Archer:
Anon:
Owen:
Clara:
Garrett:
Garrett Take 2:
Ryan:
Samuel:
Maliyah
Maddox
Adele:
Kylexa:
↧
Triumphant Tuesday: Breastfeeding After Breast Cancer
By breastfeeding her baby, a mother is giving life. She is literally keeping her child alive through the power of her body. However, what if the mother's life is in danger? Surely being faced with a breast tumour would excuse a mother from breastfeeding duties? To this mother, it was a matter of priorities, and she prioritised her baby. This is Amanda's story.
“I'll put it out there...and own it. In America, we are not a breastfeeding society. We know the research has proven breast milk to be superior over formula, but still the idea of breastfeeding gives a lot of people the heebie jeebies. While I was pregnant I was bombarded with stories about how difficult and painful breastfeeding was, and how a lot of people tried but never even made it out of the starting gate. At the same time, everyone and their dog would ask me if I planned on breastfeeding. Some people would ask multiple times.
My answer was always the same, "I'm going to try, but if it doesn't work out for me and my family then it is no big deal to use formula." (All the self described "crunchy" moms are probably throwing up in their mouths as they read that). I didn't want to set myself up for disappointment and frankly what difference was it to me whether the little sea monkey in my belly drank milk from nature’s tap or milk from a bottle?
Birth overshadowed by pessimism
When my son was born, it suddenly made a difference. Seeing him struggle to latch on, while listening to a chorus of nurses tell me that he might not be able to breastfeed and I didn't have enough colostrum, devastated me in a way I could have never anticipated. I at least wanted to be given the option to breastfeed.
Those first few days in the hospital were a roller coaster of emotions. After speaking with a lactation consultant I discovered that I did have colostrum after all...those nurses were idiots..but my son had difficulty latching and my boobs struggled to keep up with my baby walrus' increasing demands.
I was outfitted with all sorts of alien devices to help the process: nipple shields, a breast pump, collection containers, etc. Overwhelmed was the understatement of the century. I had no idea that breastfeeding could be THAT complex.
Every time I hooked those breast flanges up and started pumping, I felt like Bessie the freaking cow. Honestly, that happens to this day! I'm not sure my boobs will ever be viewed as sexual objects again. They've become a sort of freaky sideshow act. "Look how far I can shoot milk out of this one babe!" But I digress..
Clogged nipple pores
Next on the menu for me was clogged nipple pores, clogged ducts, and reoccurring mastitis. For those of you who don't know, a clogged nipple pore looks a bit like a pimple.. on your actual nipple. Super hot, right? And it feels a bit like a scalding branding iron every time you go to nurse. Now, I've got your attention! Eight hundred episodes of TLC's Make Room for Baby did NOT prepare me for that shit. On the other hand, a clogged duct feels a bit like you got donkey punched in the tit. Super sore.
Mastitis
If you are lucky enough to get mastitis, the mother of all boob ailments, then you are in for a real treat! I've had it a few times now..which I'm positive equates to like six tear drops in prison. Mastitis hits you like a ton of bricks. You suddenly just don't feel right. Perhaps, you're coming down with something? A few short hours later and your boob is painted with fire-engine red stripes, you have chills, body aches, and a fever that hovers around 104. If you're anything like me, you have no idea what the f#&k is going on the first time it happens. Hmm..is my boob supposed to be swollen like a Guatemalan cantaloupe? Basically, mastitis is when the shit hits the fan. They pump you full of antibiotics, fluids, and fever reducers. If that doesn't work you have to be hospitalized. HOSPITALIZED! How hardcore is that? Breastfeeding is not for the faint-hearted. (And you thought we were all a bunch of smelly, Pansie hippies).
Despite these hurdles, breastfeeding is a bond that I knew I wanted to share with my son. There was something so beautifully primal about it. So simple. It felt right. However one day I decided to supplement with formula a few times after my son’s hungry cries got the best of me. Giving him formula made me feel like a failure. Defective. Like I was giving up on breastfeeding. Then, nature threw me a curve-ball...
Discovery of a lump
When I was trying to get my son to latch on, I noticed a lump in my breast. I mentioned it to my obgyn at the 2 week appointment. She suggested an ultrasound. I followed through with her request and when the results came through – they were inconclusive.
I was then referred to a doctor who specialised in breasts. And this is what she said:
"We're worried it might be cancer."
I didn't answer right away. What was there to say? This wasn't candid camera, some sick joke, or even a bad dream. This was my new reality. A life where I might have breast cancer. In an instant I was bombarded with horrific mental images of hospitals, chemotherapy treatments, and even tombstones. I was petrified.
My eyes misted over. I felt the weight of everyone's gaze upon me but I wasn't ready to address the elephant in the room. Instead, I found myself looking down, losing myself in the blue/grey abyss that I knew as my baby's eyes.
The squirming bundle in my arms was blissfully oblivious. My son was only a few weeks old at the time, practically brand new, and here I was contemplating a life for him,without a mommy. It didn't seem fair. As if the emotional roller coaster of new motherhood wasn't difficult enough, I now had to contend with this. I didn't feel strong enough.
After 24 years, I had finally found my calling in life. My joy. My passion. My son. And it was all crumbling out from under me. I was drowning. Encumbered by the many questions in my head, I could barely catch my breath. Why me? Why our family?
Whether unsympathetic or unaware, the doctor droned on about the medical protocol, while I bargained with my God. She told me that we would start with a core punch needle biopsy and "go from there."
While the gravity of the situation was apparent to me, I still found myself preoccupied with the baby's well being. I only caught snippets of what the doctor was saying, and they put me in a panic.
"....and I suggest that you discontinue breastfeeding immediately."
Discontinue? But, how will I feed him? How can he nurse? We had overcome so many obstacles in learning to breastfeed. Now it all seemed for naught.
Looking back, I am confident that this specialist utilized scare tactics to ensure that I underwent an extremely costly ultrasound guided needle biopsy. I didn't have any insurance at the time, and I mentioned that I would need to "shop" around because I didn't have the 2 grand just lying around. Instead of suggesting payment plans, or another doctor, the specialist tried, and succeeded, to terrify me. She told me she was pretty confident I had cancer and was wasting precious time. She stated that she simply didn't want to see my son grow up without a mother. Essentially she preyed on a young, hormonal mom.
Biopsy
Anywho, I went through with the needle guided ultrasound biopsy. The four day wait that preceded the results was agonizing. I was weepy and irritable. My nerves were frayed from living in a perpetual state of fear and I found myself lashing out at the ones I loved most
Removal of the tumor
A new doctor suggested needle biopsy again but I was emotionally drained from the whole process. I just wanted to get the whole damn tumor out of there and put this mess behind me. So we opted for a complete excision of the lump. The surgeon was hesitant because few doctors have operated on lactating breasts. However, he supported my decision to continue nursing and after a few months, the tumor was removed.
Then, I ended up getting mastitis again! I have also had to deal with complications from the ducts that were cut (an inevitable outcome). Sometimes when my milk lets down, it will balloon in that pocket where the tumor was before. I suspect it will resolve itself when my son eventually weans. I sometimes have concerns about how this will affect my nursing relationship with future babies, but I am sure I will take it in stride. One day at a time, just like I do now.
Unsupportive relatives
This would have been an easier journey with some comprehensive support. In everything else in the world, my mom is totally supportive. However, seeing my many ups and downs in trying to breastfeed, she has pushed me to quit many times. Obviously, I am HER baby so when she believed that breastfeeding was "jeopardizing my health", she was really adamant that I should give up. Other family members haven’t been super supportive either. In the beginning, my sister in law flat out told me that breastfeeding was gross and we haven't spoken about it since. I'm far too hormonal and I might just open up a can of whoop a$$!
When to wean
I tell you all this, because I'm now in a pretty comfortable place with breastfeeding. Knock on wood, we haven't had any issues of late. So now, eight months later when me and the kid finally have our shit together, people are telling me its curtain call. "You only really need to breastfeed for 6 months." "When are you planning on going until?" "You're STILL breastfeeding?"
So you mean to tell me I went an extra two months, and I didn't have to?! Damnit! Who do I talk to about a refund?
Weaning is a topic that seems to be coming up more and more these days. Apparently, everyone and their dog thinks they have a right to comment on my boobs. Seriously...there are some very judgemental poodles out there. (Insert laugh here.)
Of course I know that according to the American Academy of Pediatrics, 6 months is the minimum recommendation and 12 months is what society interprets as the "maximum." How about this...I do what I want. Yes, I'm still breastfeeding. No, I don't have an end date in sight. How about I do what works for my family, and you mind your own god damn business. :) Since when the hell did my boobs become open to your interpretation and advice anyway?
I get it. I used to be one of those people who thought it was gross and cringed at the sight of a kid old enough to walk over and plop a boob right in his own mouth. But doing time in the breastfeeding trenches has changed me a bit. I don't know if that is what will happen in this house, but it doesn't bother me as much anymore. Even if your kid is old enough to tip his hat before sauntering over and saying, "I'm a might bit thirsty mummy, could I have a bit of milk", I think it's fine. It doesn't make you a freaking deviant.
My son will be 11 months old this week, which means continued breastfeeding solidifies my status as a freak of nature in American society. I'm sure I catch more flack than the average bear, because of my giganto baby who looks like a pre-schooler. Regardless, I think this negativity and judgement is horse crap. There is no magic date circled on my calendar. We will wean, when our family sees fit.
Mothers who don’t try
I think that Moms who don't even try to breastfeed because of superficial concerns like saggy breasts, stretch marks, the inconvenience, etc are selfish cows. I'm ok with "owning" that. There is no "I" in motherhood. It is all about sacrifice. Besides, breastfeeding is the reason we have boobs in the first place!”
Amanda's Bingo Card:
Get your own Bingo Card here.
Email me with your story.
My answer was always the same, "I'm going to try, but if it doesn't work out for me and my family then it is no big deal to use formula." (All the self described "crunchy" moms are probably throwing up in their mouths as they read that). I didn't want to set myself up for disappointment and frankly what difference was it to me whether the little sea monkey in my belly drank milk from nature’s tap or milk from a bottle?
Birth overshadowed by pessimism
When my son was born, it suddenly made a difference. Seeing him struggle to latch on, while listening to a chorus of nurses tell me that he might not be able to breastfeed and I didn't have enough colostrum, devastated me in a way I could have never anticipated. I at least wanted to be given the option to breastfeed.
Those first few days in the hospital were a roller coaster of emotions. After speaking with a lactation consultant I discovered that I did have colostrum after all...those nurses were idiots..but my son had difficulty latching and my boobs struggled to keep up with my baby walrus' increasing demands.
I was outfitted with all sorts of alien devices to help the process: nipple shields, a breast pump, collection containers, etc. Overwhelmed was the understatement of the century. I had no idea that breastfeeding could be THAT complex.
Every time I hooked those breast flanges up and started pumping, I felt like Bessie the freaking cow. Honestly, that happens to this day! I'm not sure my boobs will ever be viewed as sexual objects again. They've become a sort of freaky sideshow act. "Look how far I can shoot milk out of this one babe!" But I digress..
Clogged nipple pores
Next on the menu for me was clogged nipple pores, clogged ducts, and reoccurring mastitis. For those of you who don't know, a clogged nipple pore looks a bit like a pimple.. on your actual nipple. Super hot, right? And it feels a bit like a scalding branding iron every time you go to nurse. Now, I've got your attention! Eight hundred episodes of TLC's Make Room for Baby did NOT prepare me for that shit. On the other hand, a clogged duct feels a bit like you got donkey punched in the tit. Super sore.
Mastitis
If you are lucky enough to get mastitis, the mother of all boob ailments, then you are in for a real treat! I've had it a few times now..which I'm positive equates to like six tear drops in prison. Mastitis hits you like a ton of bricks. You suddenly just don't feel right. Perhaps, you're coming down with something? A few short hours later and your boob is painted with fire-engine red stripes, you have chills, body aches, and a fever that hovers around 104. If you're anything like me, you have no idea what the f#&k is going on the first time it happens. Hmm..is my boob supposed to be swollen like a Guatemalan cantaloupe? Basically, mastitis is when the shit hits the fan. They pump you full of antibiotics, fluids, and fever reducers. If that doesn't work you have to be hospitalized. HOSPITALIZED! How hardcore is that? Breastfeeding is not for the faint-hearted. (And you thought we were all a bunch of smelly, Pansie hippies).
Despite these hurdles, breastfeeding is a bond that I knew I wanted to share with my son. There was something so beautifully primal about it. So simple. It felt right. However one day I decided to supplement with formula a few times after my son’s hungry cries got the best of me. Giving him formula made me feel like a failure. Defective. Like I was giving up on breastfeeding. Then, nature threw me a curve-ball...
Discovery of a lump
When I was trying to get my son to latch on, I noticed a lump in my breast. I mentioned it to my obgyn at the 2 week appointment. She suggested an ultrasound. I followed through with her request and when the results came through – they were inconclusive.
I was then referred to a doctor who specialised in breasts. And this is what she said:
"We're worried it might be cancer."
I didn't answer right away. What was there to say? This wasn't candid camera, some sick joke, or even a bad dream. This was my new reality. A life where I might have breast cancer. In an instant I was bombarded with horrific mental images of hospitals, chemotherapy treatments, and even tombstones. I was petrified.
My eyes misted over. I felt the weight of everyone's gaze upon me but I wasn't ready to address the elephant in the room. Instead, I found myself looking down, losing myself in the blue/grey abyss that I knew as my baby's eyes.
The squirming bundle in my arms was blissfully oblivious. My son was only a few weeks old at the time, practically brand new, and here I was contemplating a life for him,without a mommy. It didn't seem fair. As if the emotional roller coaster of new motherhood wasn't difficult enough, I now had to contend with this. I didn't feel strong enough.
After 24 years, I had finally found my calling in life. My joy. My passion. My son. And it was all crumbling out from under me. I was drowning. Encumbered by the many questions in my head, I could barely catch my breath. Why me? Why our family?
Whether unsympathetic or unaware, the doctor droned on about the medical protocol, while I bargained with my God. She told me that we would start with a core punch needle biopsy and "go from there."
While the gravity of the situation was apparent to me, I still found myself preoccupied with the baby's well being. I only caught snippets of what the doctor was saying, and they put me in a panic.
"....and I suggest that you discontinue breastfeeding immediately."
Discontinue? But, how will I feed him? How can he nurse? We had overcome so many obstacles in learning to breastfeed. Now it all seemed for naught.
Looking back, I am confident that this specialist utilized scare tactics to ensure that I underwent an extremely costly ultrasound guided needle biopsy. I didn't have any insurance at the time, and I mentioned that I would need to "shop" around because I didn't have the 2 grand just lying around. Instead of suggesting payment plans, or another doctor, the specialist tried, and succeeded, to terrify me. She told me she was pretty confident I had cancer and was wasting precious time. She stated that she simply didn't want to see my son grow up without a mother. Essentially she preyed on a young, hormonal mom.
Biopsy
Anywho, I went through with the needle guided ultrasound biopsy. The four day wait that preceded the results was agonizing. I was weepy and irritable. My nerves were frayed from living in a perpetual state of fear and I found myself lashing out at the ones I loved most
The results were cautiously optimistic. The Pathology report suggested a non-malignant, lactating fibroadenoma. Because the specialist was such a quack, I ended up with a terrible case of mastitis. She also pushed me from beginning to end, to quit breastfeeding my little boy. He was only weeks old! I wasn't having it. After the surgery, I pumped round the clock to try and keep my supply up. My milk was full of blood and the baby was uninterested in nursing from the affected side for about a week. But we prevailed! I was told to keep an eye on the tumor, and have another ultrasound in 6 months. When I did, the results were fishy again. They "strongly suggested that I follow-up with my physician as abnormalities had been noted in the films." As if no time had passed, I plummeted down the rabbit-hole again. The all too familiar sense of foreboding enveloped me and the haunting images came flooding back.
My once squirming bundle was now a mischievous and adventurous, 7.5 month old ball of wonderment and giggles. The thought of being separated from him, temporarily or indefinitely, hit even harder than it had the first time. I was tired of being terrorized by a clump of cells.
Removal of the tumor
A new doctor suggested needle biopsy again but I was emotionally drained from the whole process. I just wanted to get the whole damn tumor out of there and put this mess behind me. So we opted for a complete excision of the lump. The surgeon was hesitant because few doctors have operated on lactating breasts. However, he supported my decision to continue nursing and after a few months, the tumor was removed.
Then, I ended up getting mastitis again! I have also had to deal with complications from the ducts that were cut (an inevitable outcome). Sometimes when my milk lets down, it will balloon in that pocket where the tumor was before. I suspect it will resolve itself when my son eventually weans. I sometimes have concerns about how this will affect my nursing relationship with future babies, but I am sure I will take it in stride. One day at a time, just like I do now.
Unsupportive relatives
This would have been an easier journey with some comprehensive support. In everything else in the world, my mom is totally supportive. However, seeing my many ups and downs in trying to breastfeed, she has pushed me to quit many times. Obviously, I am HER baby so when she believed that breastfeeding was "jeopardizing my health", she was really adamant that I should give up. Other family members haven’t been super supportive either. In the beginning, my sister in law flat out told me that breastfeeding was gross and we haven't spoken about it since. I'm far too hormonal and I might just open up a can of whoop a$$!
When to wean
I tell you all this, because I'm now in a pretty comfortable place with breastfeeding. Knock on wood, we haven't had any issues of late. So now, eight months later when me and the kid finally have our shit together, people are telling me its curtain call. "You only really need to breastfeed for 6 months." "When are you planning on going until?" "You're STILL breastfeeding?"
So you mean to tell me I went an extra two months, and I didn't have to?! Damnit! Who do I talk to about a refund?
Weaning is a topic that seems to be coming up more and more these days. Apparently, everyone and their dog thinks they have a right to comment on my boobs. Seriously...there are some very judgemental poodles out there. (Insert laugh here.)
Of course I know that according to the American Academy of Pediatrics, 6 months is the minimum recommendation and 12 months is what society interprets as the "maximum." How about this...I do what I want. Yes, I'm still breastfeeding. No, I don't have an end date in sight. How about I do what works for my family, and you mind your own god damn business. :) Since when the hell did my boobs become open to your interpretation and advice anyway?
I get it. I used to be one of those people who thought it was gross and cringed at the sight of a kid old enough to walk over and plop a boob right in his own mouth. But doing time in the breastfeeding trenches has changed me a bit. I don't know if that is what will happen in this house, but it doesn't bother me as much anymore. Even if your kid is old enough to tip his hat before sauntering over and saying, "I'm a might bit thirsty mummy, could I have a bit of milk", I think it's fine. It doesn't make you a freaking deviant.
My son will be 11 months old this week, which means continued breastfeeding solidifies my status as a freak of nature in American society. I'm sure I catch more flack than the average bear, because of my giganto baby who looks like a pre-schooler. Regardless, I think this negativity and judgement is horse crap. There is no magic date circled on my calendar. We will wean, when our family sees fit.
Mothers who don’t try
I think that Moms who don't even try to breastfeed because of superficial concerns like saggy breasts, stretch marks, the inconvenience, etc are selfish cows. I'm ok with "owning" that. There is no "I" in motherhood. It is all about sacrifice. Besides, breastfeeding is the reason we have boobs in the first place!”
Amanda's Bingo Card:
Get your own Bingo Card here.
Email me with your story.
↧
↧
How to Deal with Your Toddler’s Public Tantrums
It’s a question I get asked often. Your toddler throws a wobbler that would put a PMS sufferer to shame; and they do so – shudder - in public! This is when you wish you’d never tutted at those women struggling around supermarkets with the child from hell. Toddlers encounter frustrations at every turn. Your child may want to do things but be unable to because she is not allowed, or because she doesn’t quite have the skills yet. Or she maybe overtired, hungry, or being exposed to environments which are over-stimulating (most shopping mall tantrums fall into this latter category). Worse still, having an audience to witness your toddler’s tantrum can put you pray to judgypants folk like me.
The good news is that public tantrums become very rare between the ages of 4 and 6 as your child develops social awareness, and so would usually be too embarrassed to start shouting in public. But what is a frazzled parent to do until then? Read on...
Deep breaths
First off, it is essential that you remain calm; they can smell fear like they can smell a Greggs sausage roll. It is all too easy to overreact in front of an audience’s watchful stares. You become so concerned about what other people are thinking, that the tantrum will probably provoke a far stronger response in you than one that takes place in your own home; and your mini Russell Crowe will clock onto this. Your anxiety will feed your toddler’s anxiety and the tantrum will escalate. With all eyes suddenly swivelled in your direction, wondering how you are going to handle things, ignoring your toddler's tantrum can be hard. Yet pretending to take no notice can often help to calm things down. By withholding your attention, you are sending a clear signal to your toddler that tantrums will not get them what they want. However ignoring doesn't come naturally, so here's my five point plan:
- Stay as calm and quiet as possible.
- Avoid commenting in any way.
- Keep your facial expressions neutral.
- Avoid eye contact.
- Avoid physical contact (aside from safety measures).
If you go down the ignoring route, it is worth remembering that in most cases your toddler's tantrum will escalate or intensify before it stops. It is therefore important to stick with it soilder. If you crumble while your toddler is upping the ante, they will naturally assume that by behaving worse, they have made you give in, which obviously sets a dangerous precedent. However, if you feel that ignoring isn't for you, try the following...
Distract
One of the most effective methods of defusing a brewing tantrum is by taking your toddler's mind off whatever has pissed them off. This is particularly effective in public, as there is usually so much going on around you. Distraction can be as simple as pretending that something amazing has just happened at the other side of the store to offering your toddler something different to play with (a small bag of unusual items should always be packed when you venture outside your fortress). You will find that once your toddler's attention has been diverted, they quickly forget whatever it was that lit their fuse. If however, your toddler's tantrum has progressed so far past the starting gate that distraction is futile, it's time to move on to the next step...
Remove
If you manage to successfully keep a lid on your emotions (a whisky in the toilet can help), it is hoped that your toddler will begin to calm down. But if your toddler is still hammering around like the Gruffalo on speed, or worse – their tantrum is moving up a level from Tazmanian Devil to THE devil, you might want to consider removing them from the situation. Maybe that means leaving a friend’s house and going home, or abandoning your supermarket shop and withdrawing to the car. If in a restaurant, the toilets may offer a more private place for your toddler to blow off steam (and for you to down a vodka or two). Sometimes just the simple act of taking your toddler away from the setting where the tantrum erupted can defuse it. Other times however, you may not be able to remove your toddler from the situation, for example, if you are in an aeroplane with the seat belt signs on. When this happens, it really is a case of just gritting your teeth and waiting for the storm to pass (whilst signalling to the air hostess that you would like a double brandy).
Debrief Inlaws
A public tantrum can be bad enough, but one in front of either your own parents or your in-laws can be even worse as you will probably feel even more scruitinized. In this circumstance, it will help to speak to the grannies about the tantrums beforehand and the various ways you are trying to deal with them. Ideally, this will stop Grandma from stepping in or offering counter-productive advice; although the receptiveness of the average mother-in-law is as temperamental as the British weather.
Hold Your Fort
Don’t be tempted to give your toddler whatever it is they want just because a public tantrum looms. Like buying Playdoh when you have a carpeted house, this seems like a good idea at the time, but causes more hardship in the long run. Stand firm, and don’t try to reason with your toddler. Reasoning is a waste of time. Telling your toddler that they can’t have a toy because you bought them a present yesterday will have as much impact as explaining to your husband why you’ve decided to switch face creams – it will fall on deaf ears. Your toddler will not listen to any form of reason or explanation in the throws of a tantrum, and will actually be incapable of hearing you if the tantrum has escalated to THE devil variety. Save the reasoning and explanations for afterwards, when your toddler has calmed down and will be more receptive.
Allies
Finally, remember that most of the people you believe to be judging you are probably parents themselves, and they have in all likelihood been through exactly the same situation. As such, any looks you get when your toddler is throwing a tantrum in public are far more likely to be knowing glances and sympathetic smiles. If they are not parents, rest assured, they will get theirs in due course, heh, heh.
Keep a Record
It can help to keep a record of your toddler’s tantrums (not very uplifting bedtime reading for sure, and certainly not one for granny’s memory box). In the relief of the tantrum ending, it is all too easy to forget exactly what occurred and any lessons you could have learnt from the situation. A record will help you document the facts – it will give you a clear picture of what is happening to your toddler. Furthermore, it can be a great bribing tool when you tell your child that you will pass the tantrum record onto Santa/Daddy/Headteacher if he doesn’t eat his peas (psyche!)
Your record could include the following information:
- What usually leads to your toddler having a tantrum?
- Where do the tantrums usually occur?
- Does it happen more around a particular person?
- How often do they last?
- Describe your child’s behaviour during a tantrum.
- Where would you place it on the tantrum spectrum?
- Describe what you typically do during the tantrum.
- How does your toddler’s tantrum make you feel.
If you’ve got particularly big balls, you could post your tantrum records up here, so we can all have a gander and compare notes.
Good luck comrade.
↧
Triumphant Tuesday: Breastfeeding Despite Separation
One of the beauties of breastfeeding is that, for its optimum functioning, it requires mother and baby to be in frequent close proximity. This has the knock-on effect of strengthening the maternal-infant bond. Everyone's a winner.
But what if mother and baby are separated for prolonged periods? A lot of moms at this point, switch to formula, passing the feeding duties to someone else. Whilst this offers short-term convenience, it has all the long-term consequences associated with formula use. The following story illustrates that separation and formula-use are not compulsory bedfellows. Separation can occur for many reasons. Sometimes the baby is ill and needs medical treatment; and sometimes the mother is ill. This mom experienced both scenarios yet carried on breastfeeding.
“Breastfeeding has become such a hot button issue in our culture that I have begun to hate all references to breastfeeding challenges. To say you had a breastfeeding challenge is the American mother’s 'Get Out of Jail Free' card. No one would dare judge you for not breastfeeding if you’ve had a challenge.
If more articles and stories were written about women who faced obstacles to breastfeeding and overcame them, they could benefit women all over the country. Instead, we have a population trained (or brainwashed if you prefer) to cut and run at the first sign of difficulty. It is often too late to correct misinformation once a woman has already had a baby because she will see it as criticism. The occasional mom will actually learn from her mistakes and not repeat them with her next child, but that’s not the norm. Since becoming a mother myself, I have heard so many different “breastfeeding didn’t work for me” stories that I could write a book. I feel armed to counter their claims because I too faced some unusual breastfeeding speed bumps.
The honeymoon phase cut short
My daughter Kathleen was born after a twenty-four hour labor and two more of pushing. I breastfed her for the first time before she was taken to be checked in the nursery. That night was one I will never forget. I snuggled next to my little angel the whole time, and she nursed repeatedly. I barely slept because I was so excited to finally be a mother. In the morning, a nurse came to take her back to the nursery to be seen by her pediatrician.
About an hour later, the doctor came in to tell us that Kathleen’s white count was too high. Basically, this meant that there was an increase in disease-fighting cells (leukocytes) circulating in my baby's blood. She had been sent to the NICU for antibiotics and the nurse’s there would call me when we could come and see her.
Until that moment I first visited my daughter in the NICU, I had no idea that IV’s could be placed in someone’s head. Kathleen had one lodged in her scalp; they even had to shave off some of her hair. Before her stint in intensive care was over, the IV would infiltrate three different times. Kathleen left the hospital with only the hair on the back of her head, but that was the least of our concerns.
The doctor’s orders were for me to be allowed in to nurse the baby in the NICU whenever necessary. They gave me a rocking chair and a pillow in a small storage room off of the main unit. Imagine learning to breastfeed on a hard chair in a tiny room, with the pressure of knowing that if you weren’t finished in a certain amount of time, they would come and get the baby.
Separation
Kathleen’s white count still wasn’t normal that Sunday, but my insurance was kicking me out. The hospital told me that I could stay until midnight. I had already discussed breastfeeding with the NICU nurses. My plan was to come back every two to three hours round the clock. My partner and my mother convinced me to skip one feeding in the middle of the night so that I could sleep, since we would have to drive to and from the hospital every time. If I had it to do again, I would probably have spent the night on the couch in the waiting room. The nurses offered to give Kathleen “gavage feeding” for that one time a night, which meant sticking a tube down her throat and into her stomach to deliver formula. The idea was to avoid nipple confusion, but I asked them to give her the formula in a bottle. After all of the needles and suffering she was already dealing with, I didn’t want to add to it with another medical procedure.
I was pumping like a fiend in the hospital. The nurses brought the big, scary double pump to me, and since I wanted her to have nothing but breastmilk, I pumped every 2-3 hours, just like they instructed me to.
At ten o’clock that Sunday night, my partner loaded my things into the car while I held and nursed our daughter. At five minutes until midnight, we buzzed Kathleen’s nurse to come and get her. That was the most horrible feeling I had ever experienced. Andy and I walked out of the room after the nurse, who was pushing our baby in her isolette. She turned right towards the NICU, and we turned left towards our car. Unlike every TV show and movie I had ever seen, no one came to wheel me out. There was no fanfare or Hallmark moment. It was like my part was over, and I had no more value. I still cannot believe that we had to drive home without our daughter, but we did. I pumped and cried myself to sleep so that I could be up at six to go back and nurse her.
The next few days were a blur. My partner drove me to and from the hospital all of the next day. The nurses were nice; they could call me if Kathleen was crying before her scheduled feeding so that we could rush over there. A few times, one of them was even holding her while they did paperwork so that she wouldn’t cry. Every night, we would get home from nursing the baby at around midnight. I would sit on the couch to pump before bed. Nothing came out. Every time I went in to nurse, they would ask me if my milk had come in. It hadn't.
Formula bullying
It wasn’t all bearable, though. On the first day of our separation, a nurse came into the little room with a bottle of formula in her hand. She told me that the doctor wanted me to give it to Kathleen before I nursed her. When I asked why, she said that the baby was jaundiced and the formula would help. Luckily for me, my mom was in the next room working. I ran out nearly crying and told her what was happening. She agreed that my milk wouldn’t come in well if the baby was already full of formula at every feeding. She told me to only offer the bottle after nursing, which I did. Kathleen didn’t even want a sip.
They also introduced the pacifier to my baby while she was there, but I didn’t complain as they were using it to soothe her when I wasn’t there to comfort her. By the next evening, I was thoroughly depressed. I was lying on my parents’ couch, waiting until it was time to go back to my baby. She was days old, and I had never changed her diaper or bathed her; she had nurses to do that for her. I think that in that moment, my strong commitment to breastfeeding was forged. I realized that if I didn’t nurse my child and provide her with a form of nourishment that only I could give, then I wasn’t really crucial to her survival. Other people could change her, hold her, rock her, and give her a bottle. I was dispensable.
Since then, I have learned even more about the importance of breastfeeding for my children’s health (both mental and physical) and my own health, but at that instant, all I thought was that this was something no one else could do for her.
When my baby eventually was allowed to come home I never gave her another bottle. She was not interested in the pacifier anymore once she was with me. Despite my challenges, I managed to exclusively breastfeed (not counting the three bottles of formula she drank in the hospital) her until she was twenty-two months old, and I was pregnant with her little brother.
Baby #2 is born
To our immense relief, Alexander was totally healthy at birth. After only a four hour labor, I began pushing. That went on for two and a half hours, and his head never engaged in my pelvis. He was “sunny-side up” as the doctor called it, and he ended up being born via a c-section. I nursed him for the first time about an hour after his birth, and we never experienced any problems. My breastfeeding challenges with my son didn’t begin until his third month.
Surgery #1
I had been diagnosed with gallstones during my pregnancy. I suffered from about nine “attacks” while I was pregnant, but managed to avoid surgery. When Alexander was three months old, I finally went to a surgeon because the problem was persisting. She told me that I would have to have laparoscopic surgery to remove my gallbladder. I immediately began researching anesthesia and breastfeeding. I used an online help form to talk to a Le Leche League expert. She sent me several articles to read. I also called the lactation consultant at the hospital to ask her advice. She was very reassuring that I would be able to nurse as soon as I wanted after the surgery.
I breastfed Alexander minutes before being wheeled away to the OR. The anesthesiologist came in to speak with me at that moment and said that he’d make sure to use meds that were safe for the baby. Alexander didn’t even miss a feeding.
Surgery #2
When he was nine months old, I found out that I would need outpatient surgery again. This time it was to drain an ovarian cyst that had developed during my pregnancy. I was nervous about the prospect of another operation, but I was confident that breastfeeding wouldn’t present any challenges. I woke up in the recovery room to a nurse who informed me that the doctor had had to make a large incision, and that I would have to stay overnight.
Malicious Nurse
I immediately thought of my baby and how I was going to nurse him. After finding out that I'd had to have my entire ovary removed, I had to deal with an idiot of a nurse who yelled at me for breastfeeding a nine month old! She shouted at me, as I cried over the loss of my ovary, in front of my parents, my three year old daughter, and my husband. The nurse seemed to sense that she was facing a resentful audience because she muttered something about the baby being able to spend the night and left. He did spend that night with me in my hospital bed.
I am happy to say that (so far) everything has gone smoothly with nursing my third baby, who is now seventeen months old. She latched on an hour after another c-section, and has been going strong ever since. I use my stories of the breastfeeding challenges I have faced not to gloat over my success, but to encourage other mothers to overcome whatever may be trying to prevent them from successfully breastfeeding their own babies. I believe that we have to stop politely nodding when a new mom says she couldn’t nurse because she had a c-section or a sick baby or sore nipples. I’ve had all three, and my children have all managed to breastfeed well into toddlerhood.”
Get your own Bingo Card here.
Email me with your story.
But what if mother and baby are separated for prolonged periods? A lot of moms at this point, switch to formula, passing the feeding duties to someone else. Whilst this offers short-term convenience, it has all the long-term consequences associated with formula use. The following story illustrates that separation and formula-use are not compulsory bedfellows. Separation can occur for many reasons. Sometimes the baby is ill and needs medical treatment; and sometimes the mother is ill. This mom experienced both scenarios yet carried on breastfeeding.
“Breastfeeding has become such a hot button issue in our culture that I have begun to hate all references to breastfeeding challenges. To say you had a breastfeeding challenge is the American mother’s 'Get Out of Jail Free' card. No one would dare judge you for not breastfeeding if you’ve had a challenge.
If more articles and stories were written about women who faced obstacles to breastfeeding and overcame them, they could benefit women all over the country. Instead, we have a population trained (or brainwashed if you prefer) to cut and run at the first sign of difficulty. It is often too late to correct misinformation once a woman has already had a baby because she will see it as criticism. The occasional mom will actually learn from her mistakes and not repeat them with her next child, but that’s not the norm. Since becoming a mother myself, I have heard so many different “breastfeeding didn’t work for me” stories that I could write a book. I feel armed to counter their claims because I too faced some unusual breastfeeding speed bumps.
The honeymoon phase cut short
My daughter Kathleen was born after a twenty-four hour labor and two more of pushing. I breastfed her for the first time before she was taken to be checked in the nursery. That night was one I will never forget. I snuggled next to my little angel the whole time, and she nursed repeatedly. I barely slept because I was so excited to finally be a mother. In the morning, a nurse came to take her back to the nursery to be seen by her pediatrician.
About an hour later, the doctor came in to tell us that Kathleen’s white count was too high. Basically, this meant that there was an increase in disease-fighting cells (leukocytes) circulating in my baby's blood. She had been sent to the NICU for antibiotics and the nurse’s there would call me when we could come and see her.
Until that moment I first visited my daughter in the NICU, I had no idea that IV’s could be placed in someone’s head. Kathleen had one lodged in her scalp; they even had to shave off some of her hair. Before her stint in intensive care was over, the IV would infiltrate three different times. Kathleen left the hospital with only the hair on the back of her head, but that was the least of our concerns.
The doctor’s orders were for me to be allowed in to nurse the baby in the NICU whenever necessary. They gave me a rocking chair and a pillow in a small storage room off of the main unit. Imagine learning to breastfeed on a hard chair in a tiny room, with the pressure of knowing that if you weren’t finished in a certain amount of time, they would come and get the baby.
Separation
Kathleen’s white count still wasn’t normal that Sunday, but my insurance was kicking me out. The hospital told me that I could stay until midnight. I had already discussed breastfeeding with the NICU nurses. My plan was to come back every two to three hours round the clock. My partner and my mother convinced me to skip one feeding in the middle of the night so that I could sleep, since we would have to drive to and from the hospital every time. If I had it to do again, I would probably have spent the night on the couch in the waiting room. The nurses offered to give Kathleen “gavage feeding” for that one time a night, which meant sticking a tube down her throat and into her stomach to deliver formula. The idea was to avoid nipple confusion, but I asked them to give her the formula in a bottle. After all of the needles and suffering she was already dealing with, I didn’t want to add to it with another medical procedure.
I was pumping like a fiend in the hospital. The nurses brought the big, scary double pump to me, and since I wanted her to have nothing but breastmilk, I pumped every 2-3 hours, just like they instructed me to.
At ten o’clock that Sunday night, my partner loaded my things into the car while I held and nursed our daughter. At five minutes until midnight, we buzzed Kathleen’s nurse to come and get her. That was the most horrible feeling I had ever experienced. Andy and I walked out of the room after the nurse, who was pushing our baby in her isolette. She turned right towards the NICU, and we turned left towards our car. Unlike every TV show and movie I had ever seen, no one came to wheel me out. There was no fanfare or Hallmark moment. It was like my part was over, and I had no more value. I still cannot believe that we had to drive home without our daughter, but we did. I pumped and cried myself to sleep so that I could be up at six to go back and nurse her.
The next few days were a blur. My partner drove me to and from the hospital all of the next day. The nurses were nice; they could call me if Kathleen was crying before her scheduled feeding so that we could rush over there. A few times, one of them was even holding her while they did paperwork so that she wouldn’t cry. Every night, we would get home from nursing the baby at around midnight. I would sit on the couch to pump before bed. Nothing came out. Every time I went in to nurse, they would ask me if my milk had come in. It hadn't.
Formula bullying
It wasn’t all bearable, though. On the first day of our separation, a nurse came into the little room with a bottle of formula in her hand. She told me that the doctor wanted me to give it to Kathleen before I nursed her. When I asked why, she said that the baby was jaundiced and the formula would help. Luckily for me, my mom was in the next room working. I ran out nearly crying and told her what was happening. She agreed that my milk wouldn’t come in well if the baby was already full of formula at every feeding. She told me to only offer the bottle after nursing, which I did. Kathleen didn’t even want a sip.
They also introduced the pacifier to my baby while she was there, but I didn’t complain as they were using it to soothe her when I wasn’t there to comfort her. By the next evening, I was thoroughly depressed. I was lying on my parents’ couch, waiting until it was time to go back to my baby. She was days old, and I had never changed her diaper or bathed her; she had nurses to do that for her. I think that in that moment, my strong commitment to breastfeeding was forged. I realized that if I didn’t nurse my child and provide her with a form of nourishment that only I could give, then I wasn’t really crucial to her survival. Other people could change her, hold her, rock her, and give her a bottle. I was dispensable.
Since then, I have learned even more about the importance of breastfeeding for my children’s health (both mental and physical) and my own health, but at that instant, all I thought was that this was something no one else could do for her.
When my baby eventually was allowed to come home I never gave her another bottle. She was not interested in the pacifier anymore once she was with me. Despite my challenges, I managed to exclusively breastfeed (not counting the three bottles of formula she drank in the hospital) her until she was twenty-two months old, and I was pregnant with her little brother.
Baby #2 is born
To our immense relief, Alexander was totally healthy at birth. After only a four hour labor, I began pushing. That went on for two and a half hours, and his head never engaged in my pelvis. He was “sunny-side up” as the doctor called it, and he ended up being born via a c-section. I nursed him for the first time about an hour after his birth, and we never experienced any problems. My breastfeeding challenges with my son didn’t begin until his third month.
Surgery #1
I had been diagnosed with gallstones during my pregnancy. I suffered from about nine “attacks” while I was pregnant, but managed to avoid surgery. When Alexander was three months old, I finally went to a surgeon because the problem was persisting. She told me that I would have to have laparoscopic surgery to remove my gallbladder. I immediately began researching anesthesia and breastfeeding. I used an online help form to talk to a Le Leche League expert. She sent me several articles to read. I also called the lactation consultant at the hospital to ask her advice. She was very reassuring that I would be able to nurse as soon as I wanted after the surgery.
I breastfed Alexander minutes before being wheeled away to the OR. The anesthesiologist came in to speak with me at that moment and said that he’d make sure to use meds that were safe for the baby. Alexander didn’t even miss a feeding.
Surgery #2
When he was nine months old, I found out that I would need outpatient surgery again. This time it was to drain an ovarian cyst that had developed during my pregnancy. I was nervous about the prospect of another operation, but I was confident that breastfeeding wouldn’t present any challenges. I woke up in the recovery room to a nurse who informed me that the doctor had had to make a large incision, and that I would have to stay overnight.
Malicious Nurse
I immediately thought of my baby and how I was going to nurse him. After finding out that I'd had to have my entire ovary removed, I had to deal with an idiot of a nurse who yelled at me for breastfeeding a nine month old! She shouted at me, as I cried over the loss of my ovary, in front of my parents, my three year old daughter, and my husband. The nurse seemed to sense that she was facing a resentful audience because she muttered something about the baby being able to spend the night and left. He did spend that night with me in my hospital bed.
I am happy to say that (so far) everything has gone smoothly with nursing my third baby, who is now seventeen months old. She latched on an hour after another c-section, and has been going strong ever since. I use my stories of the breastfeeding challenges I have faced not to gloat over my success, but to encourage other mothers to overcome whatever may be trying to prevent them from successfully breastfeeding their own babies. I believe that we have to stop politely nodding when a new mom says she couldn’t nurse because she had a c-section or a sick baby or sore nipples. I’ve had all three, and my children have all managed to breastfeed well into toddlerhood.”
Get your own Bingo Card here.
Email me with your story.
↧
The Laziness Conundrum
Defensive Formula Feeders (DFFs) often remark that they are seen as lazy because they chose to formula feed. One of the most common retorts to their laziness label is to argue the following:
“How can formula feeding be lazy? We have to wash and sterilise bottles, boil kettles, measure formula, carry it around, and so on; whilst all a breastfeeding mother has to do is lift her top”.
At first glance, this may seem like a worthwhile argument. After all - these things are true; formula feeding has a lot more ‘chores’ involved with it than nature’s way.
Nonetheless, I maintain that for most formula feeding mothers, laziness underlines their feeding ethos.
Here's the most common scenario:
Mother strugglers with breastfeeding, and thinks to herself, "this is too much effort, I'm switching to formula" (Grass is Greener mentality). Perhaps there is also a health professional on the scene pushing formula ‘top ups’, and formula advertising showing chubby, thriving babies.
So, rather than doing some research or seeking a second opinion (which requires effort) she switches to formula.
At first she feels liberated – she has ‘her body back’ and perhaps even a few more hours sleep as she gets someone else to exert the effort of night feeds. This help with feeding is irregular however, and within a few weeks she discovers, to her great disappointment, that formula feeding is more inconvenient that she had anticipated. Sadly by now her milk has dried up.
The sensible thing to do at this point would be to relactate, however this takes even more effort than her current situation, so she stays locked into formula feeding. Trapped in an endless cycle of washing and sterilising, feeling guilty, and defensively spouting her breastfeeding woes to whoever will listen.
What underlies the choices in this timeline of events? - laziness.
What about women who chose to formula feed from the start - they head straight to the daily sterilisation and kettle boiling rituals, so how can they be lazy for choosing the most inconvenient feeding method? A common reason you will hear from mothers who chose to formula feed from the get go (perhaps THE most common reason) is that they wanted their partner to be able to bond with the baby.
Mothers who say this don't actually believe it of course. It's a ploy to make them appear thoughtful and selfless. In reality, no sane person believes that holding a plastic teat in a baby's mouth is the only way to bond. Yet these mothers use the paternal bonding argument time and time again, as a 'get out of jail free' card. The actual motive of these mothers is that they want other people to feed their baby and they don't see why they should have to do it all themselves - laziness.
Until there is a dramatic cultural shift from prioritising parental convenient to prioritising infant need, laziness will continue to be the driving force behind most mothers’ feeding choices; and what’s more, formula companies will continue to capitalise from it.
“How can formula feeding be lazy? We have to wash and sterilise bottles, boil kettles, measure formula, carry it around, and so on; whilst all a breastfeeding mother has to do is lift her top”.
At first glance, this may seem like a worthwhile argument. After all - these things are true; formula feeding has a lot more ‘chores’ involved with it than nature’s way.
Nonetheless, I maintain that for most formula feeding mothers, laziness underlines their feeding ethos.
Here's the most common scenario:
Mother strugglers with breastfeeding, and thinks to herself, "this is too much effort, I'm switching to formula" (Grass is Greener mentality). Perhaps there is also a health professional on the scene pushing formula ‘top ups’, and formula advertising showing chubby, thriving babies.
So, rather than doing some research or seeking a second opinion (which requires effort) she switches to formula.
At first she feels liberated – she has ‘her body back’ and perhaps even a few more hours sleep as she gets someone else to exert the effort of night feeds. This help with feeding is irregular however, and within a few weeks she discovers, to her great disappointment, that formula feeding is more inconvenient that she had anticipated. Sadly by now her milk has dried up.
The sensible thing to do at this point would be to relactate, however this takes even more effort than her current situation, so she stays locked into formula feeding. Trapped in an endless cycle of washing and sterilising, feeling guilty, and defensively spouting her breastfeeding woes to whoever will listen.
What underlies the choices in this timeline of events? - laziness.
What about women who chose to formula feed from the start - they head straight to the daily sterilisation and kettle boiling rituals, so how can they be lazy for choosing the most inconvenient feeding method? A common reason you will hear from mothers who chose to formula feed from the get go (perhaps THE most common reason) is that they wanted their partner to be able to bond with the baby.
Mothers who say this don't actually believe it of course. It's a ploy to make them appear thoughtful and selfless. In reality, no sane person believes that holding a plastic teat in a baby's mouth is the only way to bond. Yet these mothers use the paternal bonding argument time and time again, as a 'get out of jail free' card. The actual motive of these mothers is that they want other people to feed their baby and they don't see why they should have to do it all themselves - laziness.
Until there is a dramatic cultural shift from prioritising parental convenient to prioritising infant need, laziness will continue to be the driving force behind most mothers’ feeding choices; and what’s more, formula companies will continue to capitalise from it.
↧
"What Does a SAHM Do All Day?"
↧
↧
Triumphant Tuesday: Breastfeeding a Premature Baby
Never is breastfeeding more important than when a baby is premature. However studies have shown that the shorter the gestational period of the baby, the shorter the length of breastfeeding (Meier 2001; Buckley and Charles 2006). Why? One reason is that mothers are being sabotaged by the medical profession. Many of the 'techniques' used to save the lives of premature babies were developed during the 1960’s and 1970’s when breastmilk, never mind breastfeeding, wasn’t a priority in neonatal intensive care units. Unfortunately, despite what the medical profession have learned since that time about how to help mothers and babies to breastfeed, NICU’s seem to be resistant to change the way babies should be fed. This mother's story is a timely illustration of this unjustifiable state of affairs.
“Having breastfed my first two babies, I felt pretty confident when I fell pregnant again.
However, this baby was premature. Following a quick cuddle just after he was born, the doctors took him away to monitor him.
Separation
Sam was a good weight and healthy so their only initial concern was that he could feed (so why separate us?) I had said that I did not want him to have formula as I was determined to breastfeed. The medical staff simply responded, "So you hope to breastfeed, do you?", which may not sound overly negative but they never gave positive reactions to my telling them that I was going to breastfeed. I wasn't hoping to - I knew I was going to. It felt like I was being subtly undermined. Then one doctor gave the line of "Well, if we need to, we will have to give him formula". I was more than happy to express to appease their obsession with measuring intake but while we were separated, they gave him formula. I'd had a c-section so couldn't get out of bed to get to him and because it was the middle of the night, my husband had been sent home. So the doctors gave him formula behind my back, without my consent.
Baby Stops Breathing
Then Sam got ill. The next morning, when my husband went to bring Sam to me, he was told that our baby was in intensive care. Sam had stopped breathing in the night and needed to be resuscitated. I hadn't been informed of his deterioration - my husband had to tell me everything. We weren't even told the whole truth and it was only recently that we found out exactly what happened to him that night. I was confused and incredibly scared. Sam had a pneumothorax and I was not allowed to hold him or feed him for 8 days. He was locked into an intensive care incubator and needed a machine to breath for him. He had all sorts of wires coming in and out of his body and I genuinely did not know whether he was going to make it or not. I was told not to touch him too much as it could cause him to be even more distressed, so I just sat there, looking at him through his the incubator glass, hoping that everything would be ok. This was about 12 hours after he had been born and I'd had a c-section so I relied on my husband to wheelchair me around. I bought a pump and expressed every 3 hours day and night.
Tube Fed
Once he was able to start having milk, Sam was tube fed for the first few days then moved onto a cup when he got a bit stronger (using my expressed breast milk of course). Eventually, we were able to achieve one successful latch per day. The staff kept telling me "We can't let him go home with you unless he's feeding properly and it's difficult to see what he's having if he's breastfeeding, whereas if he had a bottle, he could go home". I ignored them, despite desperately wanting to take him home, as I knew that breastmilk was what he needed. After a few days of pleading with staff, they agreed to let me have a room in the ward so I could prove I could manage 24 hours of feeding him from the breast without any assistance. I did this and they duly let me take him home. Since being at home, he's been fine and 20 months later, we're still breastfeeding.
Determination
It would have been so easy to have just given up on breastfeeding, especially as we were separated for so long. I was absolutely determined that he was going to be breastfed. I'd struggled through booby traps (mastitis three times, low weight gain) due to bad advice with my 1st child so I wasn't going to give up with my 3rd. The hospital could have been a lot more supportive and it worries me that their attitude means many women give up breastfeeding when they could actually do it.”
Get your own Bingo Card here.
Email me with your story.
“Having breastfed my first two babies, I felt pretty confident when I fell pregnant again.
However, this baby was premature. Following a quick cuddle just after he was born, the doctors took him away to monitor him.
Separation
Sam was a good weight and healthy so their only initial concern was that he could feed (so why separate us?) I had said that I did not want him to have formula as I was determined to breastfeed. The medical staff simply responded, "So you hope to breastfeed, do you?", which may not sound overly negative but they never gave positive reactions to my telling them that I was going to breastfeed. I wasn't hoping to - I knew I was going to. It felt like I was being subtly undermined. Then one doctor gave the line of "Well, if we need to, we will have to give him formula". I was more than happy to express to appease their obsession with measuring intake but while we were separated, they gave him formula. I'd had a c-section so couldn't get out of bed to get to him and because it was the middle of the night, my husband had been sent home. So the doctors gave him formula behind my back, without my consent.
Baby Stops Breathing
Then Sam got ill. The next morning, when my husband went to bring Sam to me, he was told that our baby was in intensive care. Sam had stopped breathing in the night and needed to be resuscitated. I hadn't been informed of his deterioration - my husband had to tell me everything. We weren't even told the whole truth and it was only recently that we found out exactly what happened to him that night. I was confused and incredibly scared. Sam had a pneumothorax and I was not allowed to hold him or feed him for 8 days. He was locked into an intensive care incubator and needed a machine to breath for him. He had all sorts of wires coming in and out of his body and I genuinely did not know whether he was going to make it or not. I was told not to touch him too much as it could cause him to be even more distressed, so I just sat there, looking at him through his the incubator glass, hoping that everything would be ok. This was about 12 hours after he had been born and I'd had a c-section so I relied on my husband to wheelchair me around. I bought a pump and expressed every 3 hours day and night.
Tube Fed
Once he was able to start having milk, Sam was tube fed for the first few days then moved onto a cup when he got a bit stronger (using my expressed breast milk of course). Eventually, we were able to achieve one successful latch per day. The staff kept telling me "We can't let him go home with you unless he's feeding properly and it's difficult to see what he's having if he's breastfeeding, whereas if he had a bottle, he could go home". I ignored them, despite desperately wanting to take him home, as I knew that breastmilk was what he needed. After a few days of pleading with staff, they agreed to let me have a room in the ward so I could prove I could manage 24 hours of feeding him from the breast without any assistance. I did this and they duly let me take him home. Since being at home, he's been fine and 20 months later, we're still breastfeeding.
Determination
It would have been so easy to have just given up on breastfeeding, especially as we were separated for so long. I was absolutely determined that he was going to be breastfed. I'd struggled through booby traps (mastitis three times, low weight gain) due to bad advice with my 1st child so I wasn't going to give up with my 3rd. The hospital could have been a lot more supportive and it worries me that their attitude means many women give up breastfeeding when they could actually do it.”
Get your own Bingo Card here.
Email me with your story.
↧
Breastmilk Storage Bags – Modelled By Men
Conceived and executed by Monday, an ad agency based in Bangkok, Thailand, this ad campaign jumps on the male breastfeeding bandwagon ignited earlier in the year by that guy who got shunned by La Leche League. The ads depict various men from across the generations lovingly nursing babies. From ‘grandpa’ to ‘brother’ (these are the labels given to the respective ads), it appears that men do want to lend a helping hand (or in this case, breast).
However WTF has this got to do with the product? The ads are trying to sell the ‘Nanny Breast Milk Storage Bag’, yet the men are feeding the babies directly from their breasts, and as they aren’t using supplemental feeding devices, this campaign makes no sense. On first glance.
Consider the target audience – pumping mothers - and the rationale behind the ads starts to fall into place. It would appear that the aim is to equate the act of nursing with the act of giving expressed breastmilk (i.e. giving breastmilk via the bottle is on par with giving it via the breast). So by expressing your milk and storing it in these freezer bags, your husband/dad/brother can then ‘breastfeed’ for you. Yes my friends, with the help of the Nanny Breast Milk Storage Bag, your baby can get all the goodness of breast milk from Daddy. Bless. However I’ve got two issues with this ad campaign. Firstly, bottle and breast are not equals, even if they both contain breast milk. There are less advantages to bottled breastmilk than breastmilk straight from the source. Secondly, the ads tap into the tired-old assumption, that in order for men to bond with their babies, they must feed them.
↧
Diagram of a BLW Baby
↧





















































































.jpg)
.jpg)
.jpg)
.jpg)



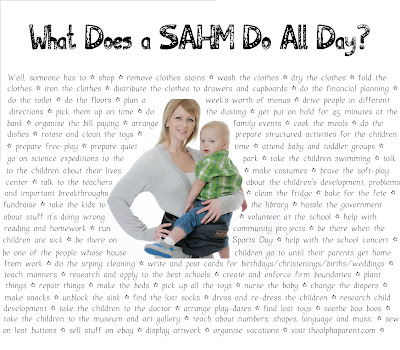


.jpg)





